Illustration by Marta Pucci
How effective is birth control?: The difference between using a method perfectly and typically

Most people want that is good at preventing unintended pregnancy. Fortunately, all methods of birth control are better at preventing pregnancy than using no method, but some methods are better than others.
How well a method works, though, depends on many factors. It’s important to understand how these factors affect each method’s ability to prevent unintended pregnancy, and how researchers describe how well the methods work.
The research terminology
Researchers often measure how well a birth control method works in two ways: perfect-use and typical-use rates (1,2). Both of these measures describe a group’s risk of pregnancy, not an individual’s risk of pregnancy.
Also, these measures are for the first year of using a method. For example, a couple may use condoms for a year, then use the pill for a year, and then switch back to condoms. The perfect-use and typical-use rate for condoms would apply to this couple for both years they used condoms, not just the first year. However, in theory, if a couple were to use condoms for two years in a row, these rates would only apply to the first year.
For users of the implant or intrauterine devices (IUDs), these rates are for the first year after having the device placed.
Are you using Clue to track your bleeding patterns? Download the app and start today

Perfect-use (also known as efficacy)
Perfect-use describes how well a method works among a group of people if used exactly as instructed, and used every time they have sex (1).
To be a “perfect user,” a person and their partner need to use a method correctly as instructed, and use it every time they have sex.
Sometimes this measurement is called a method’s efficacy. You can think of efficacy as how well the method itself works.
Typical-use (also known as effectiveness)
Typical-use describes how well a method works among a group of people who are using the method “typically” (1).
Typical users include people who
1. Use their method correctly and every time they have sex (i.e. perfect users) 2. Use their method correctly, but who don’t use it every time they have sex 3. Use their method every time they have sex, but sometimes use it incorrectly, and 4. Neither use the method correctly nor every time they have sex.
Sometimes this measurement is called a method’s effectiveness.
Typical use rates can change over time and may be different among specific populations. For example, if people become better educated on how to use condoms, then we would expect there to be fewer pregnancies among the typical-use group. (This is why you may see different typical use rates - it depends on what year the data are from and what population is being studied. The rates we present are the most up-to-date through 2021 for research done in the United States or from clinical trials, depending on the method. Typical use estimates may vary among specific populations in the US or in other countries, but this should give you a good guideline even if you're not from the US).
How to understand perfect-use (efficacy) and typical-use (effectiveness) numbers
Perfect and typical use rates are often reported as one-year pregnancy rates among 100 heterosexual couples (1).
The difference between the perfect-use and typical-use pregnancy rates gives you an idea of how difficult a method is to use.
For example, the perfect-use pregnancy rate of male condoms is 2 pregnancies out of 100 couples over 1 year (1). But the typical-use rate is 13 pregnancies out of 100 couples over 1 year (1). This means that if a person uses condoms as instructed, they work pretty well at preventing unintended pregnancy; however, it seems many people don’t use condoms as instructed, and they are at much higher risk of unintended pregnancy.
Some methods, like the implant, are really good at preventing unintended pregnancy. Methods like this have a perfect-use rate that’s less than 1 pregnancy over 1 year for 100 couples. For example, the contraceptive implant has a perfect-use and typical-use pregnancy rate of 0.1 out of 100 couples over 1 year (1).
(This can be kind of confusing, because there’s no such thing as 0.1 couples. But try moving the decimal point one space to the right. For the contraceptive implant, for example, you can think of the rate of pregnancy as 1 pregnancy per 1,000 couples per year. In comparison, the perfect-use condom rate is 20 per 1,000 couples per year.)
How do these rates compare to not using any birth control method?
The perfect-use and typical-use rates are often compared to the pregnancy rate for couples who are not using any method of birth control. Among 100 couples who use no birth control and regularly have sex, it is expected that about 85 of the female partners will become pregnant in a year (though estimates vary) (1).
Some people are physiologically less likely or completely unable to become pregnant or get someone pregnant. A person’s ability to get pregnant decreases with age (1). People who have sex less frequently are also less likely to get pregnant.
This is why perfect-use and typical-use rates shouldn’t be interpreted as a person’s individual risk of pregnancy. For example, the phrase “a person who uses condoms correctly every time they have sex has a 2% chance of pregnancy” is not correct. A person’s individual risk of pregnancy depends on a variety of factors.
Am I a “typical user” or a “perfect user”?
What perfect-use and typical-use look like depends somewhat on the method. Also, it’s not always clear how researchers would classify some couples.
Typical and Perfect Use: Condoms
For example, let’s say we have four couples who use external (male) condoms.
Couple 1 uses condoms every time they have sex, but sometimes they get confused about which way a condom should roll down. They sometimes use condoms that they originally rolled down the wrong way instead of throwing them out. The instructions say that they should throw those condoms out and use new ones.
Typical use or perfect use? Couple 1 would be “typical users” because you should throw away a condom if you put it on incorrectly.
Couple 2 knows how to use condoms correctly, but they only use condoms during the middle of the female partner’s cycle or when the female partner thinks she might be ovulating. They aren’t using a formal method of natural birth control, but just guessing at her fertile times.
Typical use or perfect use? Couple 2 would be “typical users” because they are not using condoms every time they have sex.
Couple 3 uses condoms correctly every time they have sex. If they accidentally put the condom on the wrong way, they throw out that condom and use a different one. They make sure to keep their condoms stored correctly and check the dates on the condom monthly.
Typical use or perfect use? Couple 3 would be “perfect users” because they are using condoms every time they have sex and are using condoms correctly.
Couple 4 uses condoms and the TwoDay method of natural birth control. The couple only uses condoms when the female partner has cervical fluid that suggests ovulation.
Typical use or perfect use? Couple 4 probably wouldn’t be considered “perfect users” of the TwoDay method because they used condoms during the fertile window, which isn’t considered “perfect use” by researchers for this method. They also probably wouldn’t be considered “perfect users” of condoms, because they don’t use condoms every time they have sex. Although not “perfect users” by definition, this approach to using birth control is reasonable as long as they’re using the TwoDay method properly.
Typical and Perfect Use: Combined oral contraceptive pill (“the pill”)
Perfect-use and typical-use of hormonal methods and the copper IUD look a little different. For example, let’s look at three couples who rely on the combined oral contraceptive pill.
In Couple 1, the female partner takes her pill every day around the same time. She always makes sure to get her next pill pack at least a week before she is supposed to start using the new pack, so she always starts her new pack on time.
Typical use or perfect use? This person would be a “perfect-user” of the pill.
In Couple 2, the female partner sometimes forgets to take the pill every day. She also sometimes starts her new pill pack late.
Typical use or perfect use? This person would be a “typical user” of the pill, because she doesn’t take the pill every day and because she sometimes starts her packs late.
In Couple 3, the female partner had been using the pill for a couple of years but has recently decided to stop. She had heard that it takes a few cycles to begin ovulating again, so she and her partner don’t use another method of birth control but are still having regular sex for a month after having stopped using the pill.
Typical use or perfect use? Depending on the research study, this person may be considered a “typical user” of the pill or someone who uses no method. (Unfortunately, this user was told incorrect information about how the pill works, and is at very high risk of pregnancy. Once a person stops using the pill, they are no longer considered protected from unintended pregnancy. Most people will ovulate in the cycle after they discontinue the pill (3, 4).)
Similar to condoms, there is a big difference between the perfect use and typical use pregnancy rates for the pill. Among perfect-users, less than 1 in 100 couples will get pregnant in a year (the actual number is 0.3 couples out of 100). In contrast, the pregnancy rate is 7 out of 100 typical-use couples in a year (1).
Although the condom and the pill are great at preventing unintended pregnancy, some people may find these methods difficult to use perfectly. Some methods are easier to use perfectly because they don’t require a person to take a daily pill or to remember to buy a new pack of condoms.
Typical and Perfect Use: Implant and IUDs
The implant and intrauterine devices (IUDs) have almost exactly the same perfect-use and typical-use rates (1). That’s because once they’re placed by a healthcare provider they don’t require constant visits to the pharmacy or daily reminders.
For the implant and all types of intrauterine devices (i.e. copper and hormonal), less than 1 couple out of 100 will get pregnant in 1 year during the year following insertion (1). This is true for both typical users and perfect users. The effectiveness of these methods, particularly the IUD, decrease slightly over time, but still remain very high (1).
How effective is each birth control method?
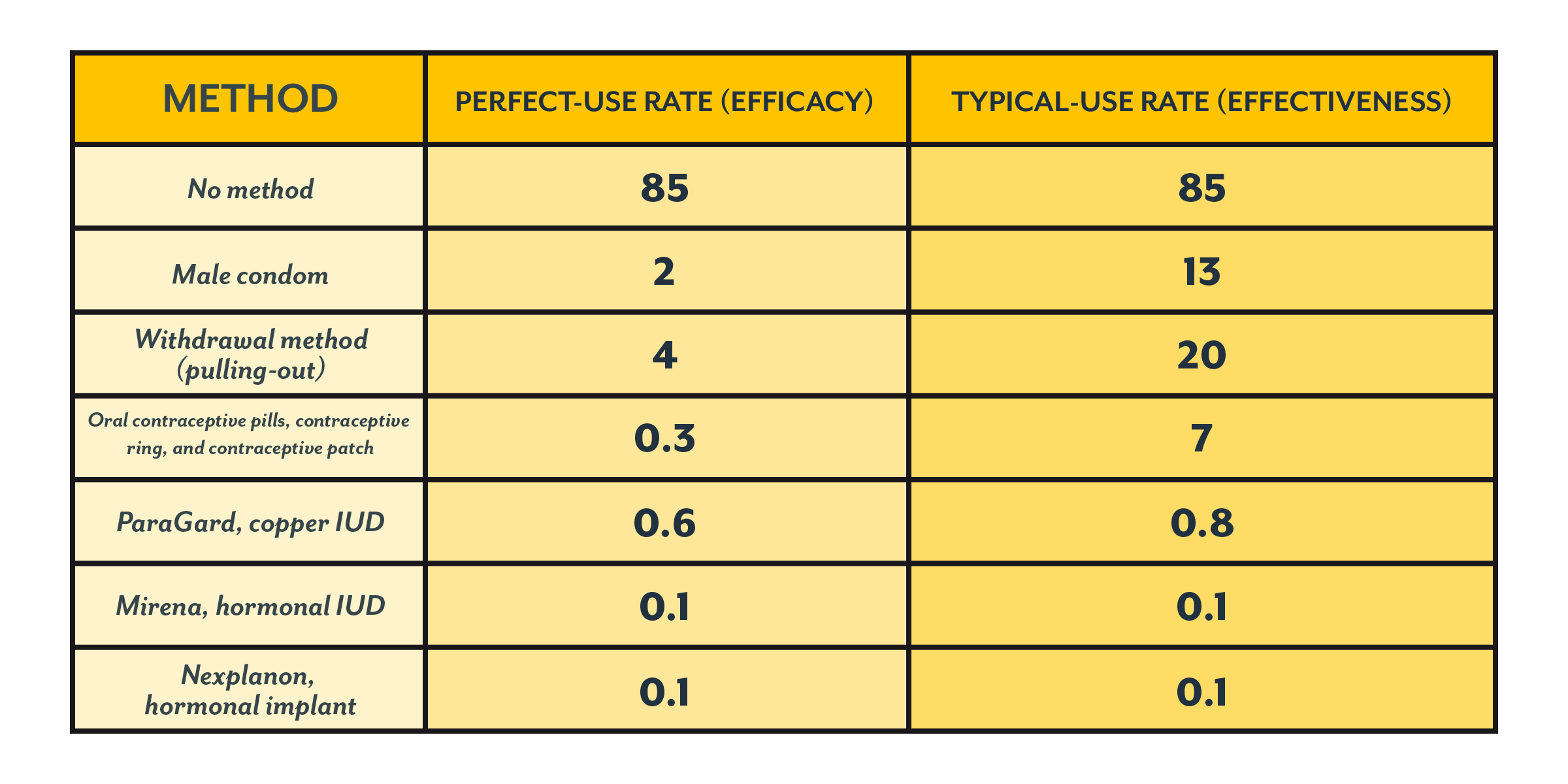
Below is a table showing the differences between the perfect-use and typical-use pregnancy rates for some methods (1). (You can compare all methods here. This is the source we used for the rates given throughout this article.)
These are the perfect-use and typical-use rates for 100 couples who use a method for one year.
Some methods, like Fertility Awareness Methods or “natural birth control” methods, are less commonly used than other forms of contraception. This can result in studies with small sample sizes, which makes it hard to generalize and to get good estimates. (We discuss some of those issues for these methods here.)
Picking a method of birth control for you
As mentioned, your risk of pregnancy is going to depend on some factors, like your age, how often you have sex, and how easy it is for you and your partner(s) to access or use your ideal form of birth control (1).
Some methods, like the withdrawal method, may be affected more by underlying physiology, whereas methods like the copper IUD work about the same in everyone. Also, people who use withdrawal and have sex often have increased risk that the withdrawer doesn’t pull out in time—whereas the number of times you have sex when using an IUD probably doesn’t matter, as long as your IUD is properly placed.
When picking a method of birth control, it’s good to look at both the perfect-use and typical-use pregnancy rates. If you think you’d be a perfect-user of a method, then the typical-use pregnancy rates probably aren’t as important for you. But it’s important to understand what it really means to be a perfect user, and typical use rates give you an idea of your risk if you have trouble being a perfect user.
What to keep in mind when talking to your healthcare provider
Although we reviewed some differences between perfect and typical users of methods here, you should talk to your healthcare provider about what constitutes perfect-use, and think about how well this method fits your life.
You can also choose to use two (or more) methods simultaneously. Correctly using multiple methods reduces the risk of unintended pregnancy further (1). For example, among 100 couples who use condoms and spermicide correctly every time they have sex over the course of one year, less than 1 couple would get pregnant (1). (Using condoms also helps prevent the spread of sexually transmitted infections.)
Of course, how well a method works may not be the only factor that matters to you. Cost, side effects, and safety concerns are often cited as important considerations in picking a birth control method (5,6). It’s important you make your concerns about methods clear to your healthcare provider.
Realistically, healthcare providers and their patients may not always agree on what’s most important. Healthcare providers may be mostly concerned with your risk of pregnancy, whereas you may be more concerned about side effects or your ability to access your method. People who are racial and/or ethnic minorities and people of lower socioeconomic status may be treated unequally by their healthcare provider (7). If your healthcare provider doesn’t seem to listen to your concerns, consider reaching out to a different provider. You deserve someone who listens to you.
Also, not all healthcare providers know how to use or teach every method of birth control. For example, natural birth control methods are often not taught to medical professionals, including obstetrician gynecologists, so they may not have the most up to date information on these methods (8-10).
Using birth control—and which form of birth control you use—is 100% your decision. Learning about yourself and about your options is the best way to reach a decision.
Clue can help you use your birth control and can be used to keep track of your sexual frequency. It also can be used to track side effects and changes to your body from birth control.
This article was originally published February 28, 2019.