Illustration by Marta Pucci
Androgens 101
Getting to know our hormones.
Hormones are so much more interesting than what we’re taught in health class. So we’ve created a guide to aaaall of the hormones. Here's everything you need to know about estrogen, progesterone, androgens, progestins, synthetic estrogen, and sex hormone binding globulin (SHBG).
What are androgens?
Simply, androgens are a group of hormones. The most well known is probably testosterone.
There are a lot of misconceptions about testosterone and other androgens. People tend to think of these as “male” hormones. It is true that testosterone is the most important hormone for sexual development of people with male sex organs (1).
That being said, all bodies—regardless of sex—produce and require some level of androgens for reproductive development (1,2).
Hormones, like androgens, facilitate communication between cells around the entire body. Some cells have androgen receptors. Think of each hormone as a key and receptors as a lock—together they make your body systems work. Hormones created from cholesterol, like androgens and estrogen, are known as steroid hormones (1).
Androgens are produced in the adrenal gland and the ovaries through the conversion of cholesterol (1,2). Muscle and fat tissue can also synthesize testosterone (3).
What do androgens do for the body?
Androgens don’t just impact our sexual health; they also play a role in our metabolism, our insulin sensitivity, and possibly our body composition (the amount and distribution of body fat and muscle)(4-6).
Androgens may also impact bone density and cardiovascular health in cis-gender women (5-7), and some research suggests that they may have an impact on brain function and mood (3,6,7), but more research is needed.
The most “important” estrogen, estradiol, is actually synthesized from testosterone by an enzyme called aromatase (1,2). Androgens also appear to impact the function of the endometrium (the lining of the uterus), and may play a role in helping prepare it to support a potential pregnancy (8).
There is also probably a relationship between libido (sexual desire) and androgen levels (3,9), but the relationship is complicated. We’ll dig deeper into this below.
How do I know if my androgen levels are normal?
Everyone has their own unique “normal.” Since “normal” changes over the course of a person’s life, symptoms may be more important than results from a hormone test. (But in case you are curious, we have also included information about typical androgen levels given by hormone tests below this section.)
Symptoms of high androgen levels include:
Hirsutism (excess hair growth)
Acne
Absent periods (amenorrhea)
Anovulation
Infertility (10,11)
Conditions that can cause or are associated with high androgen levels include:
Polycystic ovarian syndrome (PCOS)
Tumors on the adrenal gland
Tumors on the ovaries
Cushing’s disease (9,10,12)
Symptoms of low androgen levels
There are not many obvious symptoms of low androgen in cis-women and people with ovaries. Symptoms might include changes in sex drive and mood, but the research here isn’t clear cut (7,9,10).
Procedures, treatments, and conditions that can cause or are associated with unexpectedly low androgen levels include:
Primary ovarian insufficiency (i.e. very early menopause)
Surgically-induced menopause
Hypopituitarism
Chemotherapy
Adrenal insufficiency
Birth control and hormone therapy containing estrogen (7,9,10)
Some of these things can lead to low androgen levels by increasing the amount of sex hormone binding globulin (SHBG) (7,9). An increase in SHBG causes a decrease in bioavailable testosterone, so even if your total testosterone levels are normal, the testosterone that’s actually available may still be low.
Tracking your period in Clue can help you know whether your cycles are irregular.

How do androgen levels change during the menstrual cycle?
Androgen levels, like progesterone and estrogen levels, may fluctuate during the menstrual cycle. In studies of women with regular menstrual cycles, the average total testosterone among all participants peaked mid-cycle (13,14), with some studies showing a peak around the time of the luteinizing hormone surge prior to ovulation (15,16).
That being said, this may not be the case for each individual person—some people may experience multiple rises over their cycle, whereas other people’s levels may change relatively less (16). Also, some people may experience bigger relative rises than others (16).
In contrast, free testosterone (i.e. testosterone that’s more readily available for use in the body) levels might have a small peak around ovulation too, but this peak has not been shown to be statistically different from levels at other times. Also, different types of measurements find different results (13,14). This research suggests that the total testosterone (i.e. a measure all testosterone, not just readily available testosterone) peaks during the menstrual cycle may not have a noticeable effect on the body. We’ll explain why, below.
What are the types of androgens, and what do they do?
Your healthcare provider may run tests if they suspect you may have PCOS or if you have signs of high androgen levels (12). It’s important to know the different kinds of androgens that they would test for.
The most well-known androgen is testosterone, but the androgen dihydrotestosterone (DHT) is the “strongest” androgen, in that it has the biggest effect on androgen receptors (5).
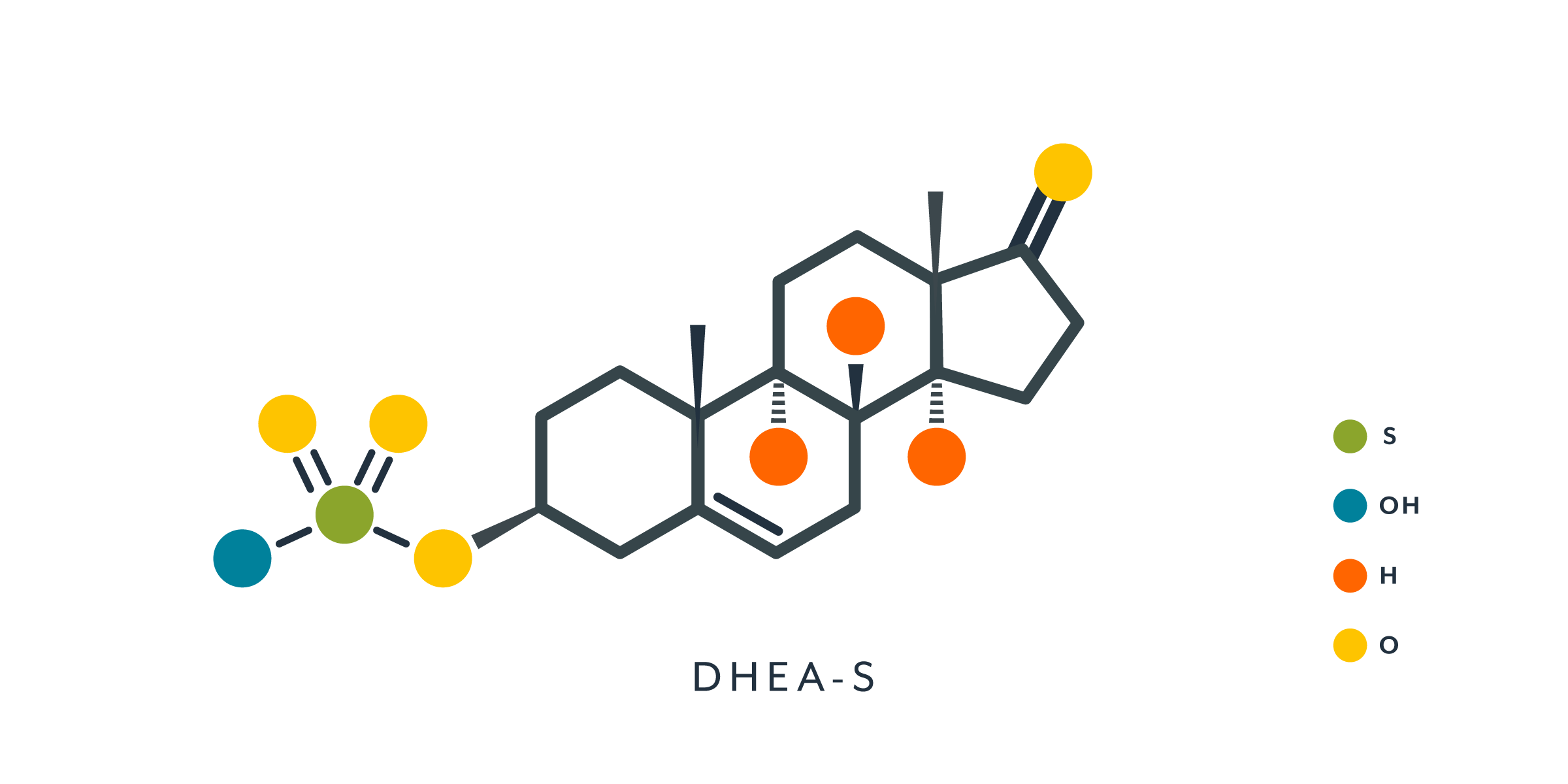
There are also a sub-class of molecules, sometimes called “pro-androgens”, because they only act weakly on androgen receptors until converted into testosterone (1,2). This sub-class includes dehydroepiandrosterone sulfate (DHEA-S), among others.
There are three types of testosterone you’ll hear about:
Total testosterone is a measure of how much testosterone is present in a blood sample (10).
Free testosterone is a measure of how much of testerone is not bonded to another molecule, either sex hormone binding globulin (SHBG) or albumin (10).
Bioavailable testosterone is a measure of free testosterone and of albumin-bonded testosterone (10).
Bioavailable testosterone and free testosterone act differently in the body than SHBG-bound testosterone (10).
Based on the levels of these three measures of testosterone, your healthcare provider may make different conclusions about the cause of your symptoms. If your total testosterone is normal, but your free testosterone is low, for instance, that may mean that you have high levels of SHBG, as opposed to low testosterone.
What are “normal” levels of androgens?
Your healthcare provider may run blood tests if they suspect you may have PCOS or if you have signs of high androgen levels (as listed above) (10-12). Knowing your levels will help your healthcare provider choose next steps.
There currently is no universal standard for diagnosing someone with clinically low androgen levels (6,7), so blood tests aren’t usually run in these scenarios.
What “normal” means can vary based on the lab you go to, where you live, your ancestry, and the testing technique. So you should always interpret your lab results with these variables in mind.
Here are reference values for testosterone and DHEA-S levels from blood samples, which are used to help diagnose some reproductive disorders (10,11).
Androgen levels between menarche and menopause
Generally, the amount of androgens in our body decreases as we age.
Total testosterone
12-16 years: less than 75 ng/dL
17-18 years: 20-75 ng/dL
> or =19 years: 8-60 ng/dL (10)
Free testosterone
For people age 15 to 18, free testosterone levels vary from <0.04-1.09 ng/dL.
After age 18, the lower bound of the normal range is 0.06 ng/dL. The upper bound of the normal range is 1.08 ng/dL for people age 19 to 24, but this value declines to 0.92 ng/dL by age 50. After a person turns 55, the upper range continues to decrease (10).
Bioavailable testosterone
< or =19 years: not established
20-50 years: 0.8-10 ng/dL
>50 Years: not established (10)
DHEA-S
12-17 years: 20-555 mcg/dL
19-30 years: 45-380 mcg/dL
31-50 years: 12-379 mcg/dL
Postmenopausal: 30-260 mcg/dL (11)
Although it’s not an androgen, someone may choose to have their SHBG levels tested if they’re worried about high androgen levels. As mentioned above, SHBG binds to testosterone. Sometimes high testosterone levels are not caused by an increase in testosterone production, but decreased levels of SHBG (2,9).
Androgen levels during pregnancy
During pregnancy, total testosterone levels increase (17,18). Levels of testosterone can also be different in different parts of the body. Testosterone levels from maternal blood, amniotic fluid, and the umbilical cord will (probably) not be the same (18).
Also, the level of testosterone in amniotic fluid (though not in maternal blood) is higher when a person is pregnant with a male fetuses (17,18).
How does hormonal birth control affect androgens?
Although hormonal contraception can lower androgen levels, the hormones in birth control also sometimes act as androgens in the body.
Some progestins—the synthetic version of the body’s natural progesterone hormone—have androgenic action (act like androgens) in the body, while others have anti-androgenic action (19). Natural progesterone is anti-androgenic (19).
Below we list different types of progestins and the birth control they are found in. The term OCs refers to oral contraceptives—birth control pills. The term combined means the pills contain estrogen.
Androgenic progestins and the types of birth control they are in:
Levonorgestrel (LNG) (hormonal IUD, combined OCs, emergency contraception pill)
Etonogestrel (contraceptive implant, vaginal ring)
(Depot) medroxyprogesterone acetate (contraceptive injection/shot)
Gestodene (combined OCs)
Desogestrel (combined OCs)
Norelgestromin (the patch)
Norethindrone and norethindrone acetate (combined OCs, progestin-only OCs) (19-22)
Anti-androgenic progestins and the types of birth control they are in:
Drospirenone (combined OCs)
Chlormadinone acetate (combined OCs)
Cyproterone acetate (combined OCs) (19-23)
Although some progestins may be more or less androgenic, this does not mean any individual person will necessarily notice high or low androgen symptoms. We discuss this more below.
Androgens and combined hormonal contraception
Combined hormonal contraception (CHC) includes all forms of birth control than contain estrogen and progestin (synthetic progesterone). CHC comes in the form of pills, a vaginal ring, and a patch that goes on your skin.
Androgens and the birth control pill
The best studied CHC is the combined oral contraceptive (OC), or “the pill.” OCs have been demonstrated to lower androgen levels, either directly or by causing an increase in SHBG (3,20,21). Their effect on androgen levels is the main reason that OCs decrease acne, treat hirsutism, and help to manage PCOS (20,24).
Different OC formulations will have different impacts on androgen levels (21,23). Also, the level to which OCs impact androgen levels may depend upon the sensitivity of androgen receptors, which can vary from person to person (25).
Androgens and the birth control ring and patch
Less research has been conducted on the ring and the patch. Studies have found that ring and OC users have lower levels of testosterone and higher levels of SHBG compared to non-users (25,26). Similar to OCs, underlying biology probably plays a role in how the ring impacts androgen levels (25).
One small study on the contraceptive patch found that patch users and combined pill users had lower free testosterone levels after three months of use. The total and free testosterone levels were similar in both groups, despite the fact that patch users had higher SHBG levels (27). The progestin in the patch was a metabolite (i.e. a broken-down form) of the progestin used in the pill, in this study (27).
Androgens and progestin-only contraception
Progestin-only forms of contraception don’t contain estrogen.
Progestin-only forms of contraception include:
hormonal intrauterine device (IUD)
the progestin-only implant
the progestin-only injection/shot (eg. DMPA)
some pills (mini-pills)
In general, we know less about how progestin-only methods impact androgens levels, but they might have an impact.
Androgens and the hormonal IUD
One study looking at the 52 mg levonorgestrel IUD found no impact on testosterone (28). Two studies found that this type of IUD lowered SHBG levels in comparison to levels before the IUD was inserted, but that the difference was not statistically significant (28,29).
Three studies did find a significant correlation between levonorgestrel levels and SHBG (28-30). If SHBG levels were high, so were levonorgestrel levels (and vice versa).
These data might suggest that different IUDs with different amounts of levonorgestrel have different effects on SHBG levels. Also, these studies might suggest that as the dosage of levonorgestrel released into the body from an IUD decreases over time, so does any impact of SHBG (if there is even a meaningful impact at all). But more research is needed before either of these ideas can be confirmed. Just because two variables are correlated doesn’t mean that one is causing the other to change.
Androgens and the birth control injection/shot
One study showed that the subcutaneous contraceptive shot with the progestin DMPA reduced total but not free testosterone after 26 weeks (two injections) of use. SHBG levels were lower after 26 weeks, which may explain why free testosterone levels were the same (31). The type of shot used in this study has a lower dose of DMPA than what most people receive, so the results might not be generalizable.
Androgens and the birth control implant
One study on the etonogestrel implant showed a significant decrease in testosterone and SHBG levels after implant insertion (32); however, there was no significant difference between testosterone levels of women not using hormonal birth control and those who were using the implant after 3 months (32). This may have been because the testerone levels in the implant group were higher than in the non-hormonal group prior to insertion. In another study, the levonorgestrel implant decreased androgen levels (33), but the authors didn’t specify which levonorgestrel implant they used in the study.
Androgens and progestin-only pills
Progestin-only pills (POPs): One study found no change in testosterone levels but a decrease in SHBG levels among levonorgestrel mini-pill users (28). We could not find any research on the mini-pill containing norethindrone.
What else should I know about androgens?
Libido (sex drive) and androgen levels
The relationship between libido (eg. sex drive) and androgen levels is complicated. Changes in libido that occur with age are thought to be caused by a decrease in androgens, particularly testosterone (3,6,9,34).
However, there does not seem to be a dose-response relationship between testosterone and libido (3,6,14,34). That is to say, people with low testosterone don’t necessarily have low libido, and people with high testosterone don’t necessarily have high libido. For example, people with PCOS tend to have high testosterone levels, but they don’t necessarily have high libidos (34,35).
It’s been suggested that measuring levels of DHEA-S would be better for identifying low libido, but more research is needed (3,9).
Furthermore, testosterone hasn’t been consistently shown to benefit premenopausal people with low libido (34), though postmenopausal people may benefit from short-term testosterone treatment (3,6). There is not a lot of research on the safety of DHEA supplementation (6).
What may be more important than absolute levels of testosterone are changes in the levels of testosterone (9,14).
But the reality is libido is affected by a lot of factors—like our overall health and how we feel about our partner (4)—so it’s not surprising that there isn’t a clear “dose-response” relationship between hormones and libido. We investigated how libido is affected, positively and negatively, by hormonal birth control here.