


A podcast about how hormones shape our world.
Latest episode:
Who you gonna call? Mythbusters!
About Hormonal
Hormones affect everyone and everything: from skin to stress to sports.
But for most of us, they're still a mystery.
Even the way we talk about hormones makes no sense. ("She's hormonal.")
So let's clear some things up. Each week, Rhea Ramjohn is asking scientists, doctors, and experts to break it all down for us.
Subscribe on your favorite platform:
Episodes
- Season 1
- Season 2

Episode 0
August 25, 2020
A Sneak Peek at Season 2
As we work hard on Season 2 of the Hormonal podcast, we’re dropping into your feed with a special request, and a small behind the...
5 min

Episode 1
October 11, 2020
Hot or not? Birth control & sex drive
How birth control affects your sexual desire, self image, and weight fluctuations.
25 min
Support Hormonal & the period tracker that’s different from the rest.
Subscribe to Clue Plus
Episode 2
October 19, 2020
The ABC: Abortion & Birth Control
What’s it like to get an abortion and the surprising ways the pandemic is changing abortion access.
34 min

Episode 3
October 26, 2020
The many sides of side effects
Hormonal birth control: positive, negative, and neutral effects
33 min
Support Hormonal & the period tracker that’s different from the rest.
Subscribe to Clue Plus
Reproductive choice and reproductive justice
with Dr. Loretta Ross
Episode 4
November 2, 2020
Reproductive choice and reproductive justice
Accessing birth control against the odds
35 min

Episode 5
November 9, 2020
Happy birthday, birth control
Controversy and celebration on the 60th anniversary of the pill
42 min


Episode 7
November 23, 2020
Risky business: birth control during COVID-19
COVID-19 is changing how we access birth control
30 min
Support Hormonal & the period tracker that’s different from the rest.
Subscribe to Clue Plus
Who you gonna call? Mythbusters!
with Lynae Brayboy, Amanda Shea & Hajnalka Hejja
Episode 8
November 30, 2020
Who you gonna call? Mythbusters!
Clue’s Science Team busts your birth control myths
37 min
Credits
Season 2
Executive Producer: Kassandra Sundt
Host: Rhea Ramjohn
Editorial Help from: Amanda Shea, Steph Liao, Nicole Leeds
Clue Design: Marta Pucci & B.J. Scheckenbach
Web Team: Yomi Eluwande, Jane Parr-Burman, Maddie Sheesley
Special Thanks: Trudie Carter, Ryan Duncan, Aubrey Bryan,
Claudia Taylor, Léna Calvarin, Lynae Brayboy
Mixing and recording help from: Bose Park Productions & Rekorder Studios in Berlin.
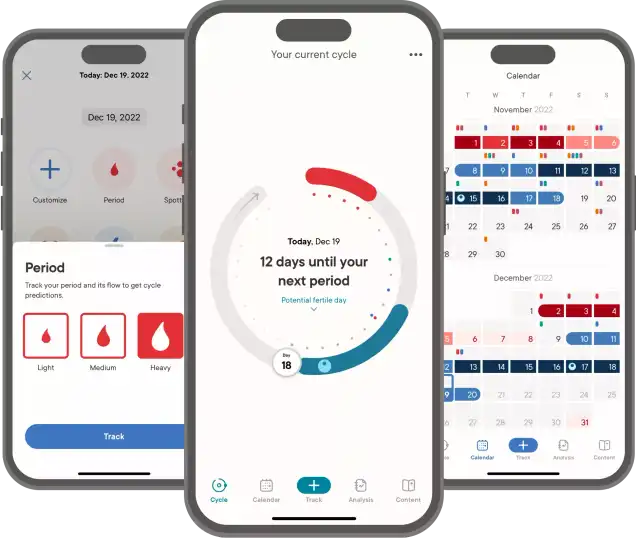
About Clue
Clue is a period tracking app that uses data and science to help women and people wih cycles to understand their bodies. It's also a menstrual and reproductive health encyclopedia.
Learn more about the Clue app and check out what Clue is doing to advance menstrual health research.


Rhea Ramjohn,
host of the Hormonal Podcast


Rhea Ramjohn,
host of the Hormonal Podcast
Your Host
The more knowledge we have about our hormones, our medical & menstrual care, and our reproductive rights, the more we empower ourselves and one another.
Hormonal has offered me the true privilege of speaking with people who have the expertise on the scientific knowledge about our hormones and cycles, as well as those sharing their lived experiences, caring for people with menstruation and how, all combined, shapes our lives everyday.
Gathering facts as well as personal stories are so vital to our understanding of our health, our his/herstories, and our cultures. I deem it a privilege because we haven't had many platforms nor opportunities for menstrual health information being broadly accessible.
Episode 8
Who you gonna call? Mythbusters!
Who you gonna call? Mythbusters!
Clue’s Science Team busts your birth control myths
About
There’s always more to learn about birth control–especially when it comes to those pesky myths that never seem to disappear. This week we’ve assembled a super squad of science-backed Mythbusters, and they tackle questions from real users like you.
Transcript
This transcript and interview were edited for clarity.
On Hormonal we explore the science behind hormones. But we also talk about society and the world around us. On Hormonal, we know that there are lots of women who have periods and lots who don’t. We also know that there are people who aren’t women who have periods too. We also know we have listeners who have never had periods. We hope you feel welcome, even when a term that a guest uses maybe doesn’t apply to you.
At Clue, we believe that our identities are not determined by our bodies. Thanks for listening to Hormonal.
Rhea Ramjohn: Hi, I'm Rhea Ramjohn, and this is Hormonal from Clue, the menstrual health app.
This season has been all about birth control, and as we reach the very last episode of the season, we wanted to touch base with our science team to answer some very important questions – questions that our Clue app users and Hormonal listeners have sent us. This is our official myth-busting episode. And here to help us bust some of these myths in this corner, I'm just kidding, but I do want to welcome back to Hormonal, Clue's Chief Medical Officer, Dr. Lynae Brayboy.
Lynae Brayboy: Hi Rhea.
Rhea Ramjohn: Hi Lynae, it's nice to have you back here.
Lynae Brayboy: Thanks.
Rhea Ramjohn: Ok, Dr. Lynae, you blew my mind in episode one with some of the facts that you laid down about sexuality and self image as it relates to hormonal birth control... so I’m hoping you can help with some of the myths sent in by our listeners.
Now let’s jump in, and hear from one of them, I appreciate so much that she called in. Here’s Grace:
Grace: “Hi, my name's Grace and I'm 15. I want to know what the best birth control is because I've been told the pill isn't the best thing to use."
Rhea Ramjohn: So, Dr. Lynae, she has heard that it's not the best thing to use. What are your thoughts about the quote unquote best form of birth control?
Lynae Brayboy: First of all, I want to say bravo, Grace, for asking the question.
Rhea Ramjohn: Absolutely.
Lynae Brayboy: But the best birth control is whatever you can take reliably, right, and so for a 15-year-old, it may not be the best thing if you can't remember to take it every single day. So the pill is something to take every single day. You can't forget it, because if you forget it, then potentially what will happen is that the hormones in the pill will not protect you from actually ovulating and therefore you could be at risk for getting pregnant. And so what we would recommend, medically speaking, is to have them take something that is long-acting and so that can be in the form of an intrauterine device that has hormones, or not. Or it can be an implant, which is actually the most effective form of birth control.
Rhea Ramjohn: And just to remind our listeners, these intrauterine devices, you said that there's one that's with hormones and there's one that isn't with hormones, right? So if I were to put myself in Grace’s position, I guess my follow up question would be, well, how does the one without hormones actually work and how effective is that?
Lynae Brayboy: Yeah, so the one with hormones, the hormone is actually called levonorgestrel, and so that hormone essentially is secreted from a device that's put into your uterus by a healthcare professional. And so if I were Grace, maybe I would think about what my bleeding is like. And if I have heavy, crampy periods, I might not want to use the one without hormones because you tend to have heavier cramping periods with the one without hormones, if that makes sense.
Rhea Ramjohn: Oh, OK. Good to know. Thank you so much for clearing that up.
Lynae Brayboy: Sure. The one with hormones actually may cause you to have a lighter period or no period at all. But it really depends on her lifestyle and her choices.
Rhea Ramjohn: OK, and kind of like the last question around this myth, she said she was told that the pill isn't the best thing to use. Any ideas, Dr. Lynae, why people have these concepts about the pill?
Lynae Brayboy: I don't know why, but I do tend to hear that people think, “Ah, the pill makes you gain weight, oh the pill does this, the pill does that.” And really, it's best that if you sit down with your healthcare practitioner and discuss the pros and cons of each method, because there is no perfect method for any one individual, you have to find out what works for you. And that's important, right?
Rhea Ramjohn: Absolutely. It's not a cookie cutter system here, right?
Lynae Brayboy: No.
Rhea Ramjohn: OK, so moving on to the next myth that we want to bust. It's from Kayley. And Kayley’s question wasn't necessarily birth control related, but wanted to know when periods become more consistent.
Kayley: My name is Kayley and I'm 14. I would love to ask, since I started my period four months ago, how long does it take for them to become regular? Thank you!
Lynae Brayboy: Right, so bravo to Kayley also for asking and being proactive about her health. So we know that once you start menses and that's called menarche, you can have a period of time for up to about two years where your menses may not be what we call, quote unquote, regular. So they may not come every 28 to 35 days. You have to find out what your pattern is. And she at this point may not know that pattern. So they start to normalize within two years because of the hypothalamic-pituitary-ovarian-axis, which actually controls the menses. So the brain speaks to the pituitary, which then speaks to the ovary and the ovary controls what happens in the uterus. That actual axis takes a little while to mature. So if you've just gotten your period four months ago, it's not quite mature. Those signals are not coming across as they should. And so you can have, what we call, irregular bleeding. And so the best thing to do is to track it, right? And, of course, Clue's a great way to track it because you're able to find out, “OK, OK, it came for the last two months, it came every 30 days. Maybe this is my pattern.” And if that pattern doesn't normalize, then definitely I would suggest Kayley and anyone else like Kayley to speak with their healthcare practitioner so they can find out, hmm, is something else going on?
Rhea Ramjohn: Right, and then how long is it that we should be tracking it before we go to our doctors and say, hey, I think that this isn't regular? What would be like a standard or a good time frame to keep in mind?
Lynae Brayboy: Well, in Kayley’s case, it's her first period, right? So it's her first year actually having menses. So we won't know what her actual pattern is like for maybe up to two years. And so she might have this irregularity that she'll have to track. But for someone who's already had regular menses that come in a predictable pattern, those individuals, if they all of a sudden become irregular, meaning they don't have a menses for over 90 days or three months, then they need to actually consult someone. Within a week if you've missed your menses and you're at risk for pregnancy, you should be thinking, “Hmmm, could I be pregnant?” Or if you don't think that you're pregnant and you have a negative pregnancy test and your menses still haven't come as they should within 90 days, you should present to your healthcare provider so they can evaluate you because it could mean something else is happening.
Rhea Ramjohn: Right. OK. I wanted to toss this next question to you because you gave us some really great advice in the first episode of the season, it was basically how to talk confidently to our doctors about our medical decisions, about what's going on in our bodies. So here’s Lucy who is 24 and sent us this question.
Lucy: I don't want kids and I know I never will. How can I confidently ask for sterilization?
Lynae Brayboy: That's right. So I think a lot of physicians especially are reluctant to offer permanent sterilization to an individual who is actually less than 30. However, if individuals have done their homework, they understand the risk so that it is permanent and cannot be reversed. And they understand that if they have a procedure where actually their tubes are removed, because now we tend to actually remove tubes and not just burn them or...
Rhea Ramjohn: Tie them?
Lynae Brayboy: Yes, I hate to say burn, but we do actually sometimes burn them. And so people understand that, oh, I can have them untied? And that's not how it works. The tube is actually damaged no matter what procedure that we do to do a tubal ligation, which again, is sort of phasing out. And we're actually now removing the tubes to decrease the risk of ovarian cancer. So if your tubes are removed or your tubes are damaged beyond repair, that's permanent, OK? And so if you need at some point, do you think you'd like to conceive, then you have to use assisted reproductive technologies such as in vitro fertilization. That's really your only option. And that can be very expensive. And so a lot of physicians are very reluctant because there will potentially be regret. Also, some insurances will not cover you for those services because you've electively or voluntarily been sterilized, if that makes sense.
Rhea Ramjohn: I always think about having autonomy over my body is really high, if not highest priority, right. And so I also value my doctor's opinion. But it's sort of strange, if I'm very honest, to have someone basically say, like, “I don't think that this is a good idea for you because you know your age and you may change your mind,” you know, it almost sounds a bit like parental.
Lynae Brayboy: Yeah, paternalistic for sure.
Rhea Ramjohn: Yeah. How is it for you as a doctor and what advice can you give to our listeners in navigating this process? In this conversation?
Lynae Brayboy: Remember that your physician is thinking of several things. So when you do a permanent sterilization procedure and someone who has a fallopian tube or fallopian tubes, rather, you essentially have to take them for a major surgery, right. And you have to put sharp instruments into their abdomen. There are risks associated with surgery: bleeding, injury to organs. And so it's not necessarily a risk-free endeavor. If there are alternatives that could achieve the same aim, then it's very likely your physician will offer you those first. And if you decide, “No, I really, really want to have this done.” I do believe that most physicians would, do believe in patient autonomy, and as long as you understand the inherent risks and benefits, then people will do it. And that has been done. It's just that, you know, I'd like our listeners to know that it's a complicated topic. It's a complicated issue because also things change. And so people feel sometimes that they weren't appropriately counseled. And so I think it's important that if this is something that Lucy wants to do or people like Lucy want to do, they should make sure that they understand and convey that they understand to their healthcare practitioner that they understand this is permanent and there are safer forms of permanent sterilization, for instance, if Lucy has a life partner, that person can also be sterilized, right? If that person is male. And that is actually a much less risky procedure.
Rhea Ramjohn: Right, specifically we’re talking about a vasectomy here, and I’m just wondering, is that procedure reversible?
Lynae Brayboy: Actually, I think people are counseled, if you are an individual with testes and vas deferens, that that procedure is also permanent. But there are surgeries that can reverse it. But depending on the age and the quality of the sperm, it may not be the best thing to do.
Rhea Ramjohn: OK, so let's say Lucy came to you and she said, I am really 100% sure I know exactly what it is I want and what I don't want. What's the best way for Lucy to get the doctor basically on her side to understand how confident she is in her decision?
Lynae Brayboy: First of all, I don't think Lucy has to get the doctor on her side. I think most physicians are just trying to make sure that they have conveyed the information. And once they've conveyed the information and the patient understands and the patient signs informed consent, which means they understand the risks and the benefits, then there's nothing else to be done except to do the surgery. So it's not a matter of getting the physician on your side. It's a matter of conveying that you truly understand there will be no natural way for you to become pregnant, that this is permanent and should not be seen as reversible. And that they are OK with the risks of surgery.
Rhea Ramjohn: Wow, OK, that's a really good point, Dr. Lynae. And thank you so much for clearing that up for us. Those were three good myths that you just busted out for us today. But I also understand that there are some other members of the Clue science team who are with us, right?
Lynae Brayboy: That's right!
Rhea Ramjohn: So that's pretty exciting, but as you know, because we follow our current regulations around here in Berlin, Germany, we can't all be in this confined studio at the same time. So let's take a short break and we’ll introduce everyone to some more members of the clue science team in a moment.
Hormonal is brought to you by Clue. The period tracking app, and menstrual health encyclopedia, and now, a pregnancy tracker!
You heard that correctly! Clue is launching our most requested feature ever: Clue Pregnancy mode! Now, you can track your pregnancy symptoms, get scientifically-backed information on how your body is changing each week, and follow your baby’s growth from conception to birth to post pregnancy.
If you’ve been using Clue as a period tracker, all you need to do is subscribe to Clue Plus, go to settings, and switch to Clue Pregnancy mode. Clue Pregnancy mode is available on Android today, and coming to Apple devices by the end of 2020.
Rhea Ramjohn: You're listening to Hormonal, I'm Rhea Ramjohn. This is our myth busting episode, and now we're joined in the studio by Clue's Head of Science, Dr. Amanda Shea. Amanda, welcome.
Amanda Shea: Hi. Thanks for having me.
Rhea Ramjohn: Well, thanks for being here. I am so excited to get your perspective because yours is a bit different from Dr. Brayboy's, because I understand you're a different kind of doctor, right?
Amanda Shea: Correct. So I'm not a medical doctor, but I do have a PhD, and my background is in ovarian cancer research.
Rhea Ramjohn: Oh, wow. And I understand you've also been at Clue for a while now, so I'm sure you come across myths all the time. So before we get into our listener questions, are there any myths that you really want to bust? You hear them so often?
Amanda Shea: Yes. And that is the myth of the 28-day cycle, which drives me crazy.
Rhea Ramjohn: Oh, wait, it's not 28 days? That’s what I've been told my entire life.
Amanda Shea: Exactly. It feels like it's constantly being reinforced that we should have an exactly 28-day cycle that comes at the exact day we expect, month after month after month. And then it's completely not true. Typical cycles can range anywhere from about 24 to 38 days and variation across cycles is completely normal. So if your period comes a few days early or a few days late from time to time, this is part of healthy functioning.
Rhea Ramjohn: Yeah. I mean it makes sense now that I think about it, we're all unique so our cycles should be unique too, right?
Amanda Shea: Of course.
Rhea Ramjohn: All right. Let's hop into these user questions. So we've had a few about PCOS and this one is from Aranza.
Aranza: Hello, my name is Aranza. I'm 22 years old and I'm from Canada. And I have a question about my birth control. I take the pill, I've been taking it for seven months now, but I'm really worried about my fertility because I have PCOS. So I would like to know how this affects taking the pill, PCOS with my fertility. Thank you.
Amanda Shea: So, Aranza, your question really has two different parts. So let's first talk about fertility and birth control, and then about PCOS. So whether a hormonal birth control negatively impacts your fertility is an extremely common question. And the truth is that most people who stop taking hormonal birth control do become pregnant within one year of trying. So after two years, if you look at people who stop taking hormonal birth control versus those who stop taking other methods like condoms, there's virtually no difference in how long it takes them to become pregnant. Now, when you stop taking the pill, it can take a few months for your cycles to come back to what they were before you started taking it. But most people do become pregnant within about eight months. So research suggests that a little over half of people conceive within three months after stopping, about 75% conceive within six months, and about 94% conceive within 12 months. So really, this is not something to worry about.
Now let's go to the part on PCOS.
Amanda Shea: So PCOS, or polycystic ovary syndrome, is an endocrine or a hormone disorder that's associated with unpredictable periods. So in people with PCOS, ovulation can occur infrequently, which then leads to having unpredictable periods. So everyone's case of PCOS is a bit different with different symptoms. So it's best to talk to your healthcare provider about your specific case and what type of birth control might be best for you.
Rhea Ramjohn: Let's keep with this topic of PCOS, because our listeners actually had a lot of questions about it. Here’s 25 year old Carmilla.
Carmilla: Does birth control really solve polycystic ovary syndrome?
Amanda Shea: That is a great question. So far, there's no known cure for PCOS, but there are various ways to manage the different symptoms associated with PCOS. So hormonal birth control, such as the pill, doesn't cure PCOS, but it can be prescribed as a first line treatment as long as you're not trying to get pregnant. Some of the symptoms that are associated with PCOS are unpredictable periods and also something called hyperandrogenism. This is when you have much higher levels of hormones, such as testosterone that are more common in men usually, and they can lead to symptoms like thinning of hair in your head, but also increased hair in your body or your face or even acne. So the pill can help to treat some of these symptoms. But it's also important to note that because PCOS is linked to various different aspects of your health, such as, as I mentioned, your different hormone levels, but also your metabolism, you might be recommended different treatment options, such as some lifestyle changes or dietary changes or even other medications such as diabetes medicine. As I said before, it's best to talk to your doctor about your specific symptoms and what birth control method might be best for you.
Rhea Ramjohn: Hmm. All right. Thanks for clearing that up for us, and I'm pretty sure all of our listeners are really happy that you busted those myths for them. So thank you so much, Amanda.
Amanda Shea: It was my pleasure.
Rhea Ramjohn Amanda Shea is Head of Science here at Clue. Thank you for joining us today. And we're going to be joined by one more science team member. So we're going to do a little swap and be back right after the break.
Hormonal is brought to you by Clue. The period tracking app and menstrual health encyclopedia that takes your cycle seriously.
Clue has been around since 2012, and since then our community has grown to millions of people. And we want to be around for years to come.
But to do that, we need support from people like you. By subscribing to Clue Plus, you’re supporting the work here at Clue. You’re also keeping the app free for others, who maybe don't have the same resources or access as you. And you’re helping fund important menstrual health research around the world.
To learn more about becoming a Clue Plus subscriber, go to Clue.plus.
Alright, back to the show.
Rhea Ramjohn: You're listening to Hormonal, I'm Rhea Ramjohn, I'm joined in the studio by our final clue expert, Dr. Hajnalka Hejja is the Science Lead for Product. Hajnalka, welcome.
Hajnalka Hejja: Hi Rhea, it's great to be here.
Rhea Ramjohn: So I understand that your job at Clue is to bring the science lense to the app, right?
Hajnalka Hejja: That is right. So what I do is that when there are practical questions on how to make Clue better for our users, I bring scientific principles into that decision making.
Rhea Ramjohn: Oh, very important part, because we definitely want to make our listeners and our users happy. So let's start with my favorite question from today's chats, which is what is a myth that you hear often and you would like to bust?
Hajnalka Hejja: OK, so you hear it often that you can't get pregnant while you are on your period, and that is not true. What is true is that you are rather unlikely to get pregnant due to the fact that ovulation, your ovary releasing the egg, happens 10, 16 days before your next period. However, in case you have a short cycle like, let's say, 24 days, it's possible that you ovulate quite close to the start date of your period. You also have to count with the fact that sperm can stay alive up to five days in the female genital tract and would be able to fertilize an egg.
Rhea Ramjohn: Oh, OK. That does make things a bit tricky then.
Hajnalka Hejja: Yeah. So therefore, unprotected sex during your period is not completely safe from getting pregnant.
Rhea Ramjohn: That’s such critical information, thank you Hajnalka.
OK, moving on to Reema, Reema's 27 and sent in this question:
Reema: Is there an increased risk of heart attack with the pill? My aunt passed away from a heart attack and everyone blamed the pill.
Rhea Ramjohn: Hajnalka, what are your thoughts on this?
Hajnalka Hejja: Yeah, first off, I'm very sorry about your Aunt, Reema. And of course, without knowing the details, I cannot really say exactly what happened to her. I can say that, generally speaking, contraceptives are safe for most people. Taking birth control is usually safer than pregnancy itself. That being said, there are benefits and risks to each type of birth control, including both side effects and the chance of a rare but serious outcome like the one that you mentioned. Heart disease, however, is the number one killer of women. Risk factors for heart disease include high blood pressure, high cholesterol, and smoking. So heart attacks are an extremely rare side effect of hormonal contraception. Smoking while using hormonal contraception greatly increases the risk of a heart attack. It's risky for smokers, especially over 35 years old, to use a combination or contraceptive pills, a commonly used type of birth control. But there are other options available, including IUDs, the implant, and the shot. And you always have to consider that, yes, everybody is unique and every birth control option will have specific risks and benefits based on your health, your age, and your own risk factors as well.
Rhea Ramjohn: I appreciate you bringing up this very important topic for our listeners, because this is something we touched on and talked about in season one of Hormonal that in the past at least, there was an increased risk of a heart attack and blood clots listed as possible side effects of hormonal birth control. So, Hajnalka, what's the science say today about the risk that we should all be aware of?
Hajnalka Hejja: Yeah. So first of all, when we talk about side effects, there's something that you have to be aware of. That's when you're taking a drug – there is no drug that has no side effects, right. However, side effects can be positive and negative as well. So, the most common negative side effects of the pill are bleeding between the period, sore breasts, nausea, or headaches. However, positive side effects could be a more regular menstrual cycle, less pain while you are on your period, reduce cancer risk, or ovarian cysts prevention. So there are quite a number of things that can be positive when you are taking a contraceptive pill.
Rhea Ramjohn: OK. Thank you so much for that. We have one more question actually about side effects. So Freyda, age 25 wrote to us to ask:
Freyda: Is it possible that localized hormone treatments such as the vaginal ring will have less severe side effects than the pill?
Hajnalka Hejja: The ring is a soft, flexible piece of plastic that's inserted into the vagina. It works primarily by suppressing ovulation, but also makes cervical mucus thicker, which makes it more difficult for sperm to cross that barrier. So let's talk about what you mean by localized. In the case of the ring, this means that the hormones from the ring are absorbed through the walls of the vagina and they act directly on your reproductive system with only a small amount of hormones making it to your bloodstream. This is different to the pill, which we call 'systemic,' because you swallow the pill and hormones travel through your whole body. The way the hormones are delivered through the vagina, it increases what we call 'bioavailability', or how much of these hormones your body can actually use. Because of this, you do not need as much of the hormone to have the same effect. So with less hormones than an oral method, it's true that some people experience fewer side effects.
Rhea Ramjohn: Right, that makes sense. Now, you explained it that way. This is exactly why I love talking to the science team at Clue, because you just break it all down and make it seem not so mysterious after all.
Hajnalka Hejja: We have a great team here.
Rhea Ramjohn Yes, we do. So, Dr. Hajnalka Hejja, Science Lead for Product and hormonal myth buster extraordinaire. Thank you for being such an informative myth buster today on the podcast.
Hajnalka Hejja: Thank you.
Rhea Ramjohn: We’ll be back right after the break.
Hormonal is brought to you by Clue. The period tracking app and menstrual health encyclopedia that takes your cycle seriously.
And right now, we’re asking for your help. Clue needs your financial support to keep the lights on. You can do that by becoming a Clue Plus subscriber. Your subscription not only keeps the work here at Clue going, but it also supports menstrual health research around the world, and protects data privacy.
Your subscription gives you access to our entire library of articles as well as new articles, app features, and curated content as they’re released.
For more on how to support the work and reap the benefits of becoming a Clue Plus subscriber, check out Clue.plus.
Alright, back to the show.
Rhea Ramjohn: You're listening to Hormonal, brought to you by Clue, the menstrual health app. I'm Rhea Ramjohn. So let's bring Dr. Lynae back in. Dr. Lynae, can you hear me?
Lynae Brayboy: Yes, I'm here.
Rhea Ramjohn: Okay, great. Well, Dr. Lynae, we have had not only some great myth busting this episode, but actually this entire season. I mean, we had the privilege of having you for our first episode as our first guest. And since then, I've learned so much from not only the side effects of birth control and the birth of the birth control pill, but I've also learned about reproductive justice and the very first experiments. I mean, really fascinating, important stuff to know about our history.
So, I would like to step back for just a second and look at the big picture here. Since you were our first guest for the first episode and you're here for our final episode, I thought you'd be the perfect person to ask: what do these conversations that we've been having all season from the history to the reproductive justice, to the side effects of the birth control pill and birth control in general, what does this say about how birth control, in all its forms, is working and also not working for us?
Lynae Brayboy: The birth control pill, the evolution of it has done so much for people with periods to be able to control whether or not they want to have children, how they want to have children, and I think that that has allowed us to do many things.
And so, I still think that birth control and its evolution has been very important. But I think in the modern times, a lot of individuals who now have delayed childbearing then actually end up seeking fertility services with reproductive endocrinologists and infertility specialists such as myself. And they do feel oftentimes that they weren't told about their menses, they weren't told how to understand their menstrual cycle. They don't understand their bodies. And in some ways, I don't fault the birth control for that, but I do fault the conversation that happens when people actually start the birth control method that they choose, right?
Rhea Ramjohn: Right. I'm really grateful that we're able to have these conversations and that you're always pushing for these very open and honest and confident conversations and especially with our health care providers. So I thank you, but I have my own little question, my own little myth that I'd like to bust.
Lynae Brayboy: Do you?
Rhea Ramjohn: Yeah, I don't know if it's so much busting a myth, but I guess I'm curious about the morning-after pill, that's a form of birth control and, I actually, it is for a friend, I'm not kidding.
Lynae Brayboy: You're asking for a friend?
Rhea Ramjohn: I'm asking for a friend! It's not really me, you know, this is just a little test to see if she's listening. No, but we were having this conversation actually earlier this week about the morning-after pill and about how it may make a person's body feel, how they might actually feel. So are there any side effects, like actual side effects, or are these all just placebo effects that we have in our head, like, “Oh, I'm trying to avoid hormones. And now I take the morning after pill and I have all these hormones in my body and it's going to wreak havoc on my cycle.” Is any of that true?
Lynae Brayboy: So, I mean, obviously, everyone reacts differently, right? We're not cookie cutters, as you said earlier, your body's not a clock. So usually with the morning-after pill, which is levonorgestrel, it's marketed as different trade names, it is in many different types of contraceptives, doesn't wreak havoc, quote unquote. It's just you take it, you have a withdrawal bleed, and essentially it’s done its job. And then as soon as you stop taking it, your levels drop in your blood and things return to normal, usually. But if you find that you have to take the morning-after pill several times in a year, then you need a more reliable method. Because it may cause you distress, you may have a placebo effect, you may feel maybe increased nausea, you may vomit. And that's obviously not ideal when you're trying to take a pill that's going to prevent pregnancy.
Rhea Ramjohn: That's a good point.
Lynae Brayboy: It's over the counter in many, many places, but in some places at certain ages, it's not over the counter. And it's also pricey. So sometimes your insurance may pay for it, sometimes your insurance may not. And obviously, there are some challenges ahead about contraceptive access. So it may be better to have a long-acting reversible method that is something you can rely on and you don't have to run out to the pharmacy to get it.
Rhea Ramjohn: Well, I think that these conversations could not be more important at a better time. I really appreciate your time. I appreciate you busting out all of these myths for us so we get the facts. And I really enjoy talking to you, as always. Dr. Lynae BrayBoy, thank you so much for being here today. She's the Chief Medical Officer here at Clue. And thanks for joining us this season on Hormonal.
Lynae Brayboy: Thank you so much, Rhea. Have a good day.
Rhea Ramjohn: You too.
Rhea Ramjohn: Listeners, I want to thank you, too! To everyone who called and wrote in, thank you so, so much! We couldn’t get to every question… but you can always check out http://helloclue.com for our encyclopedia of information.
And it’s not just this episode I want to thank you for, but sticking with us this whole season. I’ve learned so much, and I hope you did too. If you enjoyed this season, please rate us five stars. It helps other people find the podcast and maybe learn a thing or two. And don’t forget to follow us on social media! You can find us @clueapp on Instagram and @clue on Twitter.
Until next time, I’m Rhea Ramjohn, and this has been Hormonal.
Credits
Rhea Ramjohn: Hormonal is hosted by me, Rhea Ramjohn! Our Executive Producer is Kassandra Sundt.
Editorial help from:
Amanda Shea
Steph Liao
Nicole Leeds
Special thanks to:
Marta Pucci
Trudie Carter
Maddie Sheesley
Ryan Duncan
Aubrey Bryan
Claudia Taylor
Léna Calvarin
Lynae Brayboy
Yomi Eluwande
And Jane Parr-Burman
Mixing and recording help from Bose Park Productions and Rekorder Studios in Berlin.
Thanks for listening to Hormonal. Please rate and subscribe, and tell a friend! Until next time, I’m Rhea Ramjohn.
Related links:
https://helloclue.com/articles/sex/the-birth-control-implant-myths-and-questions
https://helloclue.com/articles/sex/antibiotics-and-birth-control-myths-and-facts
https://helloclue.com/articles/culture/36-superstitions-about-periods-from-around-world
https://helloclue.com/articles/culture/tampons-questions-and-misconceptions
https://helloclue.com/articles/cycle-a-z/can-you-swim-on-your-period
https://helloclue.com/articles/cycle-a-z/myth-moon-phases-menstruation

Episode 8
November 30, 2020
Who you gonna call? Mythbusters!
Clue’s Science Team busts your birth control myths
About
There��’s always more to learn about birth control–especially when it comes to those pesky myths that never seem to disappear. This week we’ve assembled a super squad of science-backed Mythbusters, and they tackle questions from real users like you.
"It feels like it's constantly being reinforced that we should have an exactly 28-day cycle that comes at the exact day we expect, month after month after month. And then it's completely not true. Who you gonna call? Mythbusters!"
On Hormonal we explore the science behind hormones. But we also talk about society and the world around us. On Hormonal, we know that there are lots of women who have periods and lots who don’t. We also know that there are people who aren’t women who have periods too. We also know we have listeners who have never had periods. We hope you feel welcome, even when a term that a guest uses maybe doesn’t apply to you.
At Clue, we believe that our identities are not determined by our bodies. Thanks for listening to Hormonal.
Rhea Ramjohn: Hi, I'm Rhea Ramjohn, and this is Hormonal from Clue, the menstrual health app.
This season has been all about birth control, and as we reach the very last episode of the season, we wanted to touch base with our science team to answer some very important questions – questions that our Clue app users and Hormonal listeners have sent us. This is our official myth-busting episode. And here to help us bust some of these myths in this corner, I'm just kidding, but I do want to welcome back to Hormonal, Clue's Chief Medical Officer, Dr. Lynae Brayboy.
Lynae Brayboy: Hi Rhea.
Rhea Ramjohn: Hi Lynae, it's nice to have you back here.
Lynae Brayboy: Thanks.
Rhea Ramjohn: Ok, Dr. Lynae, you blew my mind in episode one with some of the facts that you laid down about sexuality and self image as it relates to hormonal birth control... so I’m hoping you can help with some of the myths sent in by our listeners.
Now let’s jump in, and hear from one of them, I appreciate so much that she called in. Here’s Grace:
Grace: “Hi, my name's Grace and I'm 15. I want to know what the best birth control is because I've been told the pill isn't the best thing to use."
Rhea Ramjohn: So, Dr. Lynae, she has heard that it's not the best thing to use. What are your thoughts about the quote unquote best form of birth control?
Lynae Brayboy: First of all, I want to say bravo, Grace, for asking the question.
Rhea Ramjohn: Absolutely.
Lynae Brayboy: But the best birth control is whatever you can take reliably, right, and so for a 15-year-old, it may not be the best thing if you can't remember to take it every single day. So the pill is something to take every single day. You can't forget it, because if you forget it, then potentially what will happen is that the hormones in the pill will not protect you from actually ovulating and therefore you could be at risk for getting pregnant. And so what we would recommend, medically speaking, is to have them take something that is long-acting and so that can be in the form of an intrauterine device that has hormones, or not. Or it can be an implant, which is actually the most effective form of birth control.
Rhea Ramjohn: And just to remind our listeners, these intrauterine devices, you said that there's one that's with hormones and there's one that isn't with hormones, right? So if I were to put myself in Grace’s position, I guess my follow up question would be, well, how does the one without hormones actually work and how effective is that?
Lynae Brayboy: Yeah, so the one with hormones, the hormone is actually called levonorgestrel, and so that hormone essentially is secreted from a device that's put into your uterus by a healthcare professional. And so if I were Grace, maybe I would think about what my bleeding is like. And if I have heavy, crampy periods, I might not want to use the one without hormones because you tend to have heavier cramping periods with the one without hormones, if that makes sense.
Rhea Ramjohn: Oh, OK. Good to know. Thank you so much for clearing that up.
Lynae Brayboy: Sure. The one with hormones actually may cause you to have a lighter period or no period at all. But it really depends on her lifestyle and her choices.
Rhea Ramjohn: OK, and kind of like the last question around this myth, she said she was told that the pill isn't the best thing to use. Any ideas, Dr. Lynae, why people have these concepts about the pill?
Lynae Brayboy: I don't know why, but I do tend to hear that people think, “Ah, the pill makes you gain weight, oh the pill does this, the pill does that.” And really, it's best that if you sit down with your healthcare practitioner and discuss the pros and cons of each method, because there is no perfect method for any one individual, you have to find out what works for you. And that's important, right?
Rhea Ramjohn: Absolutely. It's not a cookie cutter system here, right?
Lynae Brayboy: No.
Rhea Ramjohn: OK, so moving on to the next myth that we want to bust. It's from Kayley. And Kayley’s question wasn't necessarily birth control related, but wanted to know when periods become more consistent.
Kayley: My name is Kayley and I'm 14. I would love to ask, since I started my period four months ago, how long does it take for them to become regular? Thank you!
Lynae Brayboy: Right, so bravo to Kayley also for asking and being proactive about her health. So we know that once you start menses and that's called menarche, you can have a period of time for up to about two years where your menses may not be what we call, quote unquote, regular. So they may not come every 28 to 35 days. You have to find out what your pattern is. And she at this point may not know that pattern. So they start to normalize within two years because of the hypothalamic-pituitary-ovarian-axis, which actually controls the menses. So the brain speaks to the pituitary, which then speaks to the ovary and the ovary controls what happens in the uterus. That actual axis takes a little while to mature. So if you've just gotten your period four months ago, it's not quite mature. Those signals are not coming across as they should. And so you can have, what we call, irregular bleeding. And so the best thing to do is to track it, right? And, of course, Clue's a great way to track it because you're able to find out, “OK, OK, it came for the last two months, it came every 30 days. Maybe this is my pattern.” And if that pattern doesn't normalize, then definitely I would suggest Kayley and anyone else like Kayley to speak with their healthcare practitioner so they can find out, hmm, is something else going on?
Rhea Ramjohn: Right, and then how long is it that we should be tracking it before we go to our doctors and say, hey, I think that this isn't regular? What would be like a standard or a good time frame to keep in mind?
Lynae Brayboy: Well, in Kayley’s case, it's her first period, right? So it's her first year actually having menses. So we won't know what her actual pattern is like for maybe up to two years. And so she might have this irregularity that she'll have to track. But for someone who's already had regular menses that come in a predictable pattern, those individuals, if they all of a sudden become irregular, meaning they don't have a menses for over 90 days or three months, then they need to actually consult someone. Within a week if you've missed your menses and you're at risk for pregnancy, you should be thinking, “Hmmm, could I be pregnant?” Or if you don't think that you're pregnant and you have a negative pregnancy test and your menses still haven't come as they should within 90 days, you should present to your healthcare provider so they can evaluate you because it could mean something else is happening.
Rhea Ramjohn: Right. OK. I wanted to toss this next question to you because you gave us some really great advice in the first episode of the season, it was basically how to talk confidently to our doctors about our medical decisions, about what's going on in our bodies. So here’s Lucy who is 24 and sent us this question.
Lucy: I don't want kids and I know I never will. How can I confidently ask for sterilization?
Lynae Brayboy: That's right. So I think a lot of physicians especially are reluctant to offer permanent sterilization to an individual who is actually less than 30. However, if individuals have done their homework, they understand the risk so that it is permanent and cannot be reversed. And they understand that if they have a procedure where actually their tubes are removed, because now we tend to actually remove tubes and not just burn them or...
Rhea Ramjohn: Tie them?
Lynae Brayboy: Yes, I hate to say burn, but we do actually sometimes burn them. And so people understand that, oh, I can have them untied? And that's not how it works. The tube is actually damaged no matter what procedure that we do to do a tubal ligation, which again, is sort of phasing out. And we're actually now removing the tubes to decrease the risk of ovarian cancer. So if your tubes are removed or your tubes are damaged beyond repair, that's permanent, OK? And so if you need at some point, do you think you'd like to conceive, then you have to use assisted reproductive technologies such as in vitro fertilization. That's really your only option. And that can be very expensive. And so a lot of physicians are very reluctant because there will potentially be regret. Also, some insurances will not cover you for those services because you've electively or voluntarily been sterilized, if that makes sense.
Rhea Ramjohn: I always think about having autonomy over my body is really high, if not highest priority, right. And so I also value my doctor's opinion. But it's sort of strange, if I'm very honest, to have someone basically say, like, “I don't think that this is a good idea for you because you know your age and you may change your mind,” you know, it almost sounds a bit like parental.
Lynae Brayboy: Yeah, paternalistic for sure.
Rhea Ramjohn: Yeah. How is it for you as a doctor and what advice can you give to our listeners in navigating this process? In this conversation?
Lynae Brayboy: Remember that your physician is thinking of several things. So when you do a permanent sterilization procedure and someone who has a fallopian tube or fallopian tubes, rather, you essentially have to take them for a major surgery, right. And you have to put sharp instruments into their abdomen. There are risks associated with surgery: bleeding, injury to organs. And so it's not necessarily a risk-free endeavor. If there are alternatives that could achieve the same aim, then it's very likely your physician will offer you those first. And if you decide, “No, I really, really want to have this done.” I do believe that most physicians would, do believe in patient autonomy, and as long as you understand the inherent risks and benefits, then people will do it. And that has been done. It's just that, you know, I'd like our listeners to know that it's a complicated topic. It's a complicated issue because also things change. And so people feel sometimes that they weren't appropriately counseled. And so I think it's important that if this is something that Lucy wants to do or people like Lucy want to do, they should make sure that they understand and convey that they understand to their healthcare practitioner that they understand this is permanent and there are safer forms of permanent sterilization, for instance, if Lucy has a life partner, that person can also be sterilized, right? If that person is male. And that is actually a much less risky procedure.
Rhea Ramjohn: Right, specifically we’re talking about a vasectomy here, and I’m just wondering, is that procedure reversible?
Lynae Brayboy: Actually, I think people are counseled, if you are an individual with testes and vas deferens, that that procedure is also permanent. But there are surgeries that can reverse it. But depending on the age and the quality of the sperm, it may not be the best thing to do.
Rhea Ramjohn: OK, so let's say Lucy came to you and she said, I am really 100% sure I know exactly what it is I want and what I don't want. What's the best way for Lucy to get the doctor basically on her side to understand how confident she is in her decision?
Lynae Brayboy: First of all, I don't think Lucy has to get the doctor on her side. I think most physicians are just trying to make sure that they have conveyed the information. And once they've conveyed the information and the patient understands and the patient signs informed consent, which means they understand the risks and the benefits, then there's nothing else to be done except to do the surgery. So it's not a matter of getting the physician on your side. It's a matter of conveying that you truly understand there will be no natural way for you to become pregnant, that this is permanent and should not be seen as reversible. And that they are OK with the risks of surgery.
Rhea Ramjohn: Wow, OK, that's a really good point, Dr. Lynae. And thank you so much for clearing that up for us. Those were three good myths that you just busted out for us today. But I also understand that there are some other members of the Clue science team who are with us, right?
Lynae Brayboy: That's right!
Rhea Ramjohn: So that's pretty exciting, but as you know, because we follow our current regulations around here in Berlin, Germany, we can't all be in this confined studio at the same time. So let's take a short break and we’ll introduce everyone to some more members of the clue science team in a moment.
Hormonal is brought to you by Clue. The period tracking app, and menstrual health encyclopedia, and now, a pregnancy tracker!
You heard that correctly! Clue is launching our most requested feature ever: Clue Pregnancy mode! Now, you can track your pregnancy symptoms, get scientifically-backed information on how your body is changing each week, and follow your baby’s growth from conception to birth to post pregnancy.
If you’ve been using Clue as a period tracker, all you need to do is subscribe to Clue Plus, go to settings, and switch to Clue Pregnancy mode. Clue Pregnancy mode is available on Android today, and coming to Apple devices by the end of 2020.
Rhea Ramjohn: You're listening to Hormonal, I'm Rhea Ramjohn. This is our myth busting episode, and now we're joined in the studio by Clue's Head of Science, Dr. Amanda Shea. Amanda, welcome.
Amanda Shea: Hi. Thanks for having me.
Rhea Ramjohn: Well, thanks for being here. I am so excited to get your perspective because yours is a bit different from Dr. Brayboy's, because I understand you're a different kind of doctor, right?
Amanda Shea: Correct. So I'm not a medical doctor, but I do have a PhD, and my background is in ovarian cancer research.
Rhea Ramjohn: Oh, wow. And I understand you've also been at Clue for a while now, so I'm sure you come across myths all the time. So before we get into our listener questions, are there any myths that you really want to bust? You hear them so often?
Amanda Shea: Yes. And that is the myth of the 28-day cycle, which drives me crazy.
Rhea Ramjohn: Oh, wait, it's not 28 days? That’s what I've been told my entire life.
Amanda Shea: Exactly. It feels like it's constantly being reinforced that we should have an exactly 28-day cycle that comes at the exact day we expect, month after month after month. And then it's completely not true. Typical cycles can range anywhere from about 24 to 38 days and variation across cycles is completely normal. So if your period comes a few days early or a few days late from time to time, this is part of healthy functioning.
Rhea Ramjohn: Yeah. I mean it makes sense now that I think about it, we're all unique so our cycles should be unique too, right?
Amanda Shea: Of course.
Rhea Ramjohn: All right. Let's hop into these user questions. So we've had a few about PCOS and this one is from Aranza.
Aranza: Hello, my name is Aranza. I'm 22 years old and I'm from Canada. And I have a question about my birth control. I take the pill, I've been taking it for seven months now, but I'm really worried about my fertility because I have PCOS. So I would like to know how this affects taking the pill, PCOS with my fertility. Thank you.
Amanda Shea: So, Aranza, your question really has two different parts. So let's first talk about fertility and birth control, and then about PCOS. So whether a hormonal birth control negatively impacts your fertility is an extremely common question. And the truth is that most people who stop taking hormonal birth control do become pregnant within one year of trying. So after two years, if you look at people who stop taking hormonal birth control versus those who stop taking other methods like condoms, there's virtually no difference in how long it takes them to become pregnant. Now, when you stop taking the pill, it can take a few months for your cycles to come back to what they were before you started taking it. But most people do become pregnant within about eight months. So research suggests that a little over half of people conceive within three months after stopping, about 75% conceive within six months, and about 94% conceive within 12 months. So really, this is not something to worry about.
Now let's go to the part on PCOS.
Amanda Shea: So PCOS, or polycystic ovary syndrome, is an endocrine or a hormone disorder that's associated with unpredictable periods. So in people with PCOS, ovulation can occur infrequently, which then leads to having unpredictable periods. So everyone's case of PCOS is a bit different with different symptoms. So it's best to talk to your healthcare provider about your specific case and what type of birth control might be best for you.
Rhea Ramjohn: Let's keep with this topic of PCOS, because our listeners actually had a lot of questions about it. Here’s 25 year old Carmilla.
Carmilla: Does birth control really solve polycystic ovary syndrome?
Amanda Shea: That is a great question. So far, there's no known cure for PCOS, but there are various ways to manage the different symptoms associated with PCOS. So hormonal birth control, such as the pill, doesn't cure PCOS, but it can be prescribed as a first line treatment as long as you're not trying to get pregnant. Some of the symptoms that are associated with PCOS are unpredictable periods and also something called hyperandrogenism. This is when you have much higher levels of hormones, such as testosterone that are more common in men usually, and they can lead to symptoms like thinning of hair in your head, but also increased hair in your body or your face or even acne. So the pill can help to treat some of these symptoms. But it's also important to note that because PCOS is linked to various different aspects of your health, such as, as I mentioned, your different hormone levels, but also your metabolism, you might be recommended different treatment options, such as some lifestyle changes or dietary changes or even other medications such as diabetes medicine. As I said before, it's best to talk to your doctor about your specific symptoms and what birth control method might be best for you.
Rhea Ramjohn: Hmm. All right. Thanks for clearing that up for us, and I'm pretty sure all of our listeners are really happy that you busted those myths for them. So thank you so much, Amanda.
Amanda Shea: It was my pleasure.
Rhea Ramjohn Amanda Shea is Head of Science here at Clue. Thank you for joining us today. And we're going to be joined by one more science team member. So we're going to do a little swap and be back right after the break.
Hormonal is brought to you by Clue. The period tracking app and menstrual health encyclopedia that takes your cycle seriously.
Clue has been around since 2012, and since then our community has grown to millions of people. And we want to be around for years to come.
But to do that, we need support from people like you. By subscribing to Clue Plus, you’re supporting the work here at Clue. You’re also keeping the app free for others, who maybe don't have the same resources or access as you. And you’re helping fund important menstrual health research around the world.
To learn more about becoming a Clue Plus subscriber, go to Clue.plus.
Alright, back to the show.
Rhea Ramjohn: You're listening to Hormonal, I'm Rhea Ramjohn, I'm joined in the studio by our final clue expert, Dr. Hajnalka Hejja is the Science Lead for Product. Hajnalka, welcome.
Hajnalka Hejja: Hi Rhea, it's great to be here.
Rhea Ramjohn: So I understand that your job at Clue is to bring the science lense to the app, right?
Hajnalka Hejja: That is right. So what I do is that when there are practical questions on how to make Clue better for our users, I bring scientific principles into that decision making.
Rhea Ramjohn: Oh, very important part, because we definitely want to make our listeners and our users happy. So let's start with my favorite question from today's chats, which is what is a myth that you hear often and you would like to bust?
Hajnalka Hejja: OK, so you hear it often that you can't get pregnant while you are on your period, and that is not true. What is true is that you are rather unlikely to get pregnant due to the fact that ovulation, your ovary releasing the egg, happens 10, 16 days before your next period. However, in case you have a short cycle like, let's say, 24 days, it's possible that you ovulate quite close to the start date of your period. You also have to count with the fact that sperm can stay alive up to five days in the female genital tract and would be able to fertilize an egg.
Rhea Ramjohn: Oh, OK. That does make things a bit tricky then.
Hajnalka Hejja: Yeah. So therefore, unprotected sex during your period is not completely safe from getting pregnant.
Rhea Ramjohn: That’s such critical information, thank you Hajnalka.
OK, moving on to Reema, Reema's 27 and sent in this question:
Reema: Is there an increased risk of heart attack with the pill? My aunt passed away from a heart attack and everyone blamed the pill.
Rhea Ramjohn: Hajnalka, what are your thoughts on this?
Hajnalka Hejja: Yeah, first off, I'm very sorry about your Aunt, Reema. And of course, without knowing the details, I cannot really say exactly what happened to her. I can say that, generally speaking, contraceptives are safe for most people. Taking birth control is usually safer than pregnancy itself. That being said, there are benefits and risks to each type of birth control, including both side effects and the chance of a rare but serious outcome like the one that you mentioned. Heart disease, however, is the number one killer of women. Risk factors for heart disease include high blood pressure, high cholesterol, and smoking. So heart attacks are an extremely rare side effect of hormonal contraception. Smoking while using hormonal contraception greatly increases the risk of a heart attack. It's risky for smokers, especially over 35 years old, to use a combination or contraceptive pills, a commonly used type of birth control. But there are other options available, including IUDs, the implant, and the shot. And you always have to consider that, yes, everybody is unique and every birth control option will have specific risks and benefits based on your health, your age, and your own risk factors as well.
Rhea Ramjohn: I appreciate you bringing up this very important topic for our listeners, because this is something we touched on and talked about in season one of Hormonal that in the past at least, there was an increased risk of a heart attack and blood clots listed as possible side effects of hormonal birth control. So, Hajnalka, what's the science say today about the risk that we should all be aware of?
Hajnalka Hejja: Yeah. So first of all, when we talk about side effects, there's something that you have to be aware of. That's when you're taking a drug – there is no drug that has no side effects, right. However, side effects can be positive and negative as well. So, the most common negative side effects of the pill are bleeding between the period, sore breasts, nausea, or headaches. However, positive side effects could be a more regular menstrual cycle, less pain while you are on your period, reduce cancer risk, or ovarian cysts prevention. So there are quite a number of things that can be positive when you are taking a contraceptive pill.
Rhea Ramjohn: OK. Thank you so much for that. We have one more question actually about side effects. So Freyda, age 25 wrote to us to ask:
Freyda: Is it possible that localized hormone treatments such as the vaginal ring will have less severe side effects than the pill?
Hajnalka Hejja: The ring is a soft, flexible piece of plastic that's inserted into the vagina. It works primarily by suppressing ovulation, but also makes cervical mucus thicker, which makes it more difficult for sperm to cross that barrier. So let's talk about what you mean by localized. In the case of the ring, this means that the hormones from the ring are absorbed through the walls of the vagina and they act directly on your reproductive system with only a small amount of hormones making it to your bloodstream. This is different to the pill, which we call 'systemic,' because you swallow the pill and hormones travel through your whole body. The way the hormones are delivered through the vagina, it increases what we call 'bioavailability', or how much of these hormones your body can actually use. Because of this, you do not need as much of the hormone to have the same effect. So with less hormones than an oral method, it's true that some people experience fewer side effects.
Rhea Ramjohn: Right, that makes sense. Now, you explained it that way. This is exactly why I love talking to the science team at Clue, because you just break it all down and make it seem not so mysterious after all.
Hajnalka Hejja: We have a great team here.
Rhea Ramjohn Yes, we do. So, Dr. Hajnalka Hejja, Science Lead for Product and hormonal myth buster extraordinaire. Thank you for being such an informative myth buster today on the podcast.
Hajnalka Hejja: Thank you.
Rhea Ramjohn: We’ll be back right after the break.
Hormonal is brought to you by Clue. The period tracking app and menstrual health encyclopedia that takes your cycle seriously.
And right now, we’re asking for your help. Clue needs your financial support to keep the lights on. You can do that by becoming a Clue Plus subscriber. Your subscription not only keeps the work here at Clue going, but it also supports menstrual health research around the world, and protects data privacy.
Your subscription gives you access to our entire library of articles as well as new articles, app features, and curated content as they’re released.
For more on how to support the work and reap the benefits of becoming a Clue Plus subscriber, check out Clue.plus.
Alright, back to the show.
Rhea Ramjohn: You're listening to Hormonal, brought to you by Clue, the menstrual health app. I'm Rhea Ramjohn. So let's bring Dr. Lynae back in. Dr. Lynae, can you hear me?
Lynae Brayboy: Yes, I'm here.
Rhea Ramjohn: Okay, great. Well, Dr. Lynae, we have had not only some great myth busting this episode, but actually this entire season. I mean, we had the privilege of having you for our first episode as our first guest. And since then, I've learned so much from not only the side effects of birth control and the birth of the birth control pill, but I've also learned about reproductive justice and the very first experiments. I mean, really fascinating, important stuff to know about our history.
So, I would like to step back for just a second and look at the big picture here. Since you were our first guest for the first episode and you're here for our final episode, I thought you'd be the perfect person to ask: what do these conversations that we've been having all season from the history to the reproductive justice, to the side effects of the birth control pill and birth control in general, what does this say about how birth control, in all its forms, is working and also not working for us?
Lynae Brayboy: The birth control pill, the evolution of it has done so much for people with periods to be able to control whether or not they want to have children, how they want to have children, and I think that that has allowed us to do many things.
And so, I still think that birth control and its evolution has been very important. But I think in the modern times, a lot of individuals who now have delayed childbearing then actually end up seeking fertility services with reproductive endocrinologists and infertility specialists such as myself. And they do feel oftentimes that they weren't told about their menses, they weren't told how to understand their menstrual cycle. They don't understand their bodies. And in some ways, I don't fault the birth control for that, but I do fault the conversation that happens when people actually start the birth control method that they choose, right?
Rhea Ramjohn: Right. I'm really grateful that we're able to have these conversations and that you're always pushing for these very open and honest and confident conversations and especially with our health care providers. So I thank you, but I have my own little question, my own little myth that I'd like to bust.
Lynae Brayboy: Do you?
Rhea Ramjohn: Yeah, I don't know if it's so much busting a myth, but I guess I'm curious about the morning-after pill, that's a form of birth control and, I actually, it is for a friend, I'm not kidding.
Lynae Brayboy: You're asking for a friend?
Rhea Ramjohn: I'm asking for a friend! It's not really me, you know, this is just a little test to see if she's listening. No, but we were having this conversation actually earlier this week about the morning-after pill and about how it may make a person's body feel, how they might actually feel. So are there any side effects, like actual side effects, or are these all just placebo effects that we have in our head, like, “Oh, I'm trying to avoid hormones. And now I take the morning after pill and I have all these hormones in my body and it's going to wreak havoc on my cycle.” Is any of that true?
Lynae Brayboy: So, I mean, obviously, everyone reacts differently, right? We're not cookie cutters, as you said earlier, your body's not a clock. So usually with the morning-after pill, which is levonorgestrel, it's marketed as different trade names, it is in many different types of contraceptives, doesn't wreak havoc, quote unquote. It's just you take it, you have a withdrawal bleed, and essentially it’s done its job. And then as soon as you stop taking it, your levels drop in your blood and things return to normal, usually. But if you find that you have to take the morning-after pill several times in a year, then you need a more reliable method. Because it may cause you distress, you may have a placebo effect, you may feel maybe increased nausea, you may vomit. And that's obviously not ideal when you're trying to take a pill that's going to prevent pregnancy.
Rhea Ramjohn: That's a good point.
Lynae Brayboy: It's over the counter in many, many places, but in some places at certain ages, it's not over the counter. And it's also pricey. So sometimes your insurance may pay for it, sometimes your insurance may not. And obviously, there are some challenges ahead about contraceptive access. So it may be better to have a long-acting reversible method that is something you can rely on and you don't have to run out to the pharmacy to get it.
Rhea Ramjohn: Well, I think that these conversations could not be more important at a better time. I really appreciate your time. I appreciate you busting out all of these myths for us so we get the facts. And I really enjoy talking to you, as always. Dr. Lynae BrayBoy, thank you so much for being here today. She's the Chief Medical Officer here at Clue. And thanks for joining us this season on Hormonal.
Lynae Brayboy: Thank you so much, Rhea. Have a good day.
Rhea Ramjohn: You too.
Rhea Ramjohn: Listeners, I want to thank you, too! To everyone who called and wrote in, thank you so, so much! We couldn’t get to every question… but you can always check out http://helloclue.com for our encyclopedia of information.
And it’s not just this episode I want to thank you for, but sticking with us this whole season. I’ve learned so much, and I hope you did too. If you enjoyed this season, please rate us five stars. It helps other people find the podcast and maybe learn a thing or two. And don’t forget to follow us on social media! You can find us @clueapp on Instagram and @clue on Twitter.
Until next time, I’m Rhea Ramjohn, and this has been Hormonal.
Credits
Rhea Ramjohn: Hormonal is hosted by me, Rhea Ramjohn! Our Executive Producer is Kassandra Sundt.
Editorial help from:
Amanda Shea
Steph Liao
Nicole Leeds
Special thanks to:
Marta Pucci
Trudie Carter
Maddie Sheesley
Ryan Duncan
Aubrey Bryan
Claudia Taylor
Léna Calvarin
Lynae Brayboy
Yomi Eluwande
And Jane Parr-Burman
Mixing and recording help from Bose Park Productions and Rekorder Studios in Berlin.
Thanks for listening to Hormonal. Please rate and subscribe, and tell a friend! Until next time, I’m Rhea Ramjohn.
Related links:
https://helloclue.com/articles/sex/the-birth-control-implant-myths-and-questions
https://helloclue.com/articles/sex/antibiotics-and-birth-control-myths-and-facts
https://helloclue.com/articles/culture/36-superstitions-about-periods-from-around-world
https://helloclue.com/articles/culture/tampons-questions-and-misconceptions
https://helloclue.com/articles/cycle-a-z/can-you-swim-on-your-period
https://helloclue.com/articles/cycle-a-z/myth-moon-phases-menstruation