


A podcast about how hormones shape our world.
Latest episode:
Who you gonna call? Mythbusters!
About Hormonal
Hormones affect everyone and everything: from skin to stress to sports.
But for most of us, they're still a mystery.
Even the way we talk about hormones makes no sense. ("She's hormonal.")
So let's clear some things up. Each week, Rhea Ramjohn is asking scientists, doctors, and experts to break it all down for us.
Subscribe on your favorite platform:
Episodes
- Season 1
- Season 2

Episode 0
August 25, 2020
A Sneak Peek at Season 2
As we work hard on Season 2 of the Hormonal podcast, we’re dropping into your feed with a special request, and a small behind the...
5 min

Episode 1
October 11, 2020
Hot or not? Birth control & sex drive
How birth control affects your sexual desire, self image, and weight fluctuations.
25 min
Support Hormonal & the period tracker that’s different from the rest.
Subscribe to Clue Plus
Episode 2
October 19, 2020
The ABC: Abortion & Birth Control
What’s it like to get an abortion and the surprising ways the pandemic is changing abortion access.
34 min

Episode 3
October 26, 2020
The many sides of side effects
Hormonal birth control: positive, negative, and neutral effects
33 min
Support Hormonal & the period tracker that’s different from the rest.
Subscribe to Clue Plus
Reproductive choice and reproductive justice
with Dr. Loretta Ross
Episode 4
November 2, 2020
Reproductive choice and reproductive justice
Accessing birth control against the odds
35 min

Episode 5
November 9, 2020
Happy birthday, birth control
Controversy and celebration on the 60th anniversary of the pill
42 min


Episode 7
November 23, 2020
Risky business: birth control during COVID-19
COVID-19 is changing how we access birth control
30 min
Support Hormonal & the period tracker that’s different from the rest.
Subscribe to Clue Plus
Who you gonna call? Mythbusters!
with Lynae Brayboy, Amanda Shea & Hajnalka Hejja
Episode 8
November 30, 2020
Who you gonna call? Mythbusters!
Clue’s Science Team busts your birth control myths
37 min
Credits
Season 2
Executive Producer: Kassandra Sundt
Host: Rhea Ramjohn
Editorial Help from: Amanda Shea, Steph Liao, Nicole Leeds
Clue Design: Marta Pucci & B.J. Scheckenbach
Web Team: Yomi Eluwande, Jane Parr-Burman, Maddie Sheesley
Special Thanks: Trudie Carter, Ryan Duncan, Aubrey Bryan,
Claudia Taylor, Léna Calvarin, Lynae Brayboy
Mixing and recording help from: Bose Park Productions & Rekorder Studios in Berlin.
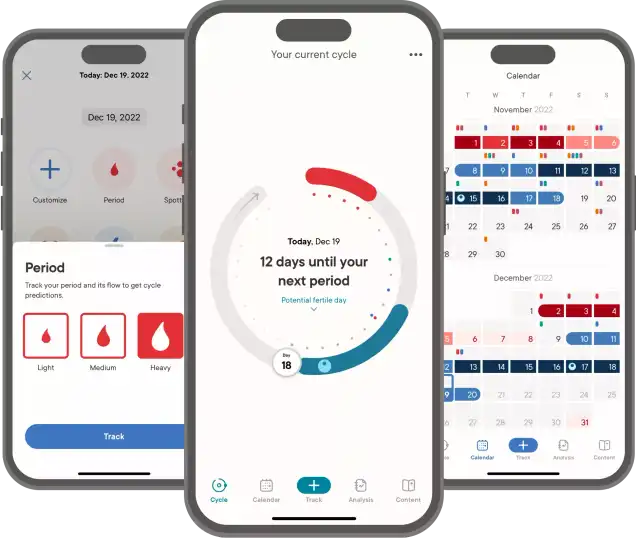
About Clue
Clue is a period tracking app that uses data and science to help women and people wih cycles to understand their bodies. It's also a menstrual and reproductive health encyclopedia.
Learn more about the Clue app and check out what Clue is doing to advance menstrual health research.


Rhea Ramjohn,
host of the Hormonal Podcast


Rhea Ramjohn,
host of the Hormonal Podcast
Your Host
The more knowledge we have about our hormones, our medical & menstrual care, and our reproductive rights, the more we empower ourselves and one another.
Hormonal has offered me the true privilege of speaking with people who have the expertise on the scientific knowledge about our hormones and cycles, as well as those sharing their lived experiences, caring for people with menstruation and how, all combined, shapes our lives everyday.
Gathering facts as well as personal stories are so vital to our understanding of our health, our his/herstories, and our cultures. I deem it a privilege because we haven't had many platforms nor opportunities for menstrual health information being broadly accessible.
Episode 2
The ABC: Abortion & Birth Control
The ABC: Abortion & Birth Control
What’s it like to get an abortion and the surprising ways the pandemic is changing abortion access.
About
1 in 4 people capable of getting pregnant will have an abortion in their lifetime. Despite this, finding accurate information about abortions is tricky. That’s why we’re exploring this topic and the stigma around it in our latest episode of Hormonal.
Transcript
This transcript and interview were edited for clarity.
What’s it like to get an abortion and the surprising ways the pandemic is changing abortion access.
This episode of Hormonal is brought to you with financial support from Bayer. To learn more about Bayer’s support of Hormonal and other work here at Clue, check out helloclue.com/bayer.
On Hormonal, we explore the science behind hormones. But we also talk about society and the world around us. We know that there are lots of women who have periods and lots who don’t. We also know that there are people who aren’t women who have periods too. We also know we have listeners who have never had periods. We hope you feel welcome, even when a term that a guest uses maybe doesn’t apply to you.
At Clue, we believe that our identities are not determined by our bodies and we hope you feel welcome. Thanks for listening to Hormonal.
Rhea Ramjohn: Hi, I'm Rhea Ramjohn, and you're listening to Hormonal brought to you by Clue, the menstrual health app. This season, we’re focusing on birth control.
Birth control to me, and I’m sure to many people, is really about self determination. It’s about controlling my own body, and feeling empowered in that decision. In almost all cases, when we’re talking about birth control, we’re talking about preventing conception. Things like, condoms, the pill, and IUDs. These all prevent sperm from fertilizing an egg, and implanting in the uterus.
But what about what happens after a conception does take place? While most health care providers would not consider abortion a form of birth control, it does exist in this same universe of self determination and controlling our bodies. According to the Guttmacher institute and World Health Organization, there were on average 73 million abortions every year between 2015 and 2019.
And when performed properly, an abortion is one of the safest procedures out there. But politically and socially, there is still a stigma.
So today, we’re going to talk about what people should know about terminating a pregnancy, and how access is changing.
For more, we're joined by Stephanie Frazin from San Francisco, California. She's a physician, researcher and family planning fellow and abortion expert at the University of California, San Francisco. Stephanie, welcome to Hormonal.
Stephanie Frazin: Thanks for having me.
Rhea Ramjohn: So for this episode, we are not going to be talking quite so much about spontaneous abortions. Also known as miscarriages. We're going to be talking more about people who choose to terminate their pregnancies. Frazin, as I know you also like to be called in terms of options that are out there. There are medical and surgical abortions, correct?
Stephanie Frazin: Yes.
Rhea Ramjohn: Can you tell us how these work?
Stephanie Frazin: Yeah, sure. So I'll just tell you what an experience would be for someone who comes to see me in the clinic, who doesn't want to continue their pregnancy or is considering not continuing their pregnancy. When they first come, usually we'll chat with them about how far along that they think they are. And people who are less than 10 weeks along have the choice of either what we call medication abortion, or they have the choice of having a procedure which is sometimes called a dilation and curettage or a dilation and evacuation. If someone thinks that they want to have a medication abortion, we would walk them through what to expect and give them the pills for medication abortion, the first pill for medication abortion is called mifepristone. It's a very safe medication that works against the hormone progesterone, which is a hormone that we all have in our bodies and that supports pregnancy.
The second medications are ones that they'll take at home later. That medication is called misoprostol, and that medication can help actually pass the pregnancy. If someone was interested in a medication abortion. We would also chat with them about things to expect when they go home and take that misoprostol, which is typically someone starting to have bleeding and cramping, usually within six hours after taking the medication. But sometimes it takes up to 24 hours and that bleeding can be like a period, sometimes heavier than a period. And it kind of leads up to the point of passing the pregnancy and then becomes lighter after the pregnancy is passed. And that usually coincides with cramping,//which can be managed with maybe a heating pack, like Ibuprofen.
Rhea Ramjohn: Ok, you’ve mentioned early pregnancy options. And as a reminder to listeners, you’re talking about what to expect at your clinic, but experiences and regulations around gestational age can vary between countries and even states within the same country. Now, what about as the pregnancy progresses?
Stephanie Frazin: If someone presented to our clinic and were below the gestation of 24 weeks pregnancy, then they would have the option of having a surgical or procedural abortion. Below 14 weeks, that's called a dilation and curettage or D&C, and between 14 and 24 weeks, it's called a dilation and evacuation procedure. And if someone was interested in that, I would walk them through exactly what to expect for that procedure. And that, you know, the first thing that we do is set someone up kind of as if they were going to have a pap smear, laying with their back on a table and their feet up in stirrups. We then when they're ready, you know, at our clinic, we give the option for sedation. So, for a D&C procedure, people receive sedation and then they kind of guide us, do they want more sedation to be super sleepy or do they want to be less sleepy? And then we let them tell us when they're ready to start the procedure.
Past certain gestational ages will also have an anesthesiologist involved and they can give additional sedation until the person is sleepier and we always wait until either the person tells us that they're ready to start or they're asleep, depending on what our conversation has been beforehand. Then we'll place the speculum, which is that same kind of, metal or plastic device, that is placed in the vagina for things like pap smears or other gynecological exams. And once we place the speculum, we'll get the cervix in view, clean off the cervix. And then at our clinic, we do numbing medication around the cervix until we've tested to make sure that if the person is still awake that they're comfortable and if they're not comfortable, we take more time to do more numbing medication until they feel like they're ready to start. And then we'll dilate the cervix to the appropriate amount. And the cervix is kind of this you know, it's this closed door between the vagina and the uterus. And so we gently open it with dilators that go up in size. And then once we reach the appropriate size, we enter, we introduce this little straw into the uterus and that straw is then attached to suction and is used to perform the abortion.
Rhea Ramjohn: Can you tell me, is one type of abortion more common than the other?
Stephanie Frazin: Yeah. In the United States, surgical abortion is more common than medication abortion, but medication abortion is growing in popularity for many different reasons. You know, some people choose to have medication abortions because they want to avoid having a surgical procedure. You did mention earlier that it's a very safe procedure and it is. But some people just would prefer to avoid having any instrumentation or any procedure on their uterus. Other reasons: sometimes people do it for privacy. They want to have a medication abortion in the safety and security of their home versus having it in a clinic. Other reasons why medication abortion is growing in popularity is, you know, some people feel that it feels more like a natural process. Although you are using medications, the process is very similar to if someone was experiencing a miscarriage. And the other reason why people are more commonly having medication abortions, especially right now, is because of restrictions in abortion access. And some people are even, you know, navigating the Internet and ordering medications over the Internet to be able to have a medication abortion at home without the support of a clinic or a doctor because they aren't able to access an abortion or even a medication abortion where they live.
Rhea Ramjohn: Ok, I’d like to follow up on that a little bit. Just framing it within our current times in COVID. Is that another reason why you believe the medical abortions are on the rise? That people are able to facilitate this process at home?
Stephanie Frazin: So, you know, the numbers of growing medication abortion were actually happening before COVID and going up from, you know, about 20% of people using medication for abortion previously, to the most recent was about 39% of abortions in the United States are with medication. We don't have numbers yet to see how that has changed during the pandemic. But I can tell you anecdotally, there have been more, of course, there have been more restrictions around abortion during the pandemic. And so more people we know, we just don't have an exact number, more people are accessing medication abortion, definitely. And that may be, there have been some very recent changes in restrictions around medication abortion, actually relieving some restrictions during the pandemic. Previously, that first medication that I had mentioned mifepristone, is controlled by something called the REMS criteria through the FDA. So the REMS criteria is something that controls that first medication that we talked about, mifepristone. And REMS criteria. It's kind of funny to look at the other things that it controls. It controls very toxic chemotherapeutic agents through the FDA, things that it would be unsafe for someone to touch or handle. So it's used to make sure that those medications are only given in a health care facility by a licensed provider. This also applies to mifepristone, not for safety reasons, because it's a very safe medication, but for political reasons to limit access to mifepristone for medication abortion.
Stephanie Frazin: Just two weeks ago, a judge ruled that this REMS criteria would not apply to mifepristone during the pandemic. So kind of hot off the press made this ruling that would make it so that we would be able to, as clinicians, mail the medication to people. And that way we could expand access to medication abortion for people all over the United States, even if they weren't able to physically access a provider in a clinic, which was the previous situation.
Rhea Ramjohn: Right. So, Stephanie, tell us who seeks abortions.
Stephanie Frazin: So I think each of us maybe has that thought in our mind of, you know, who is the type of person getting abortions. And as I became an abortion provider, I learned that there really is no stereotype there. There are all different people who are accessing abortion care. And the average person is someone who is already a parent and maybe making this decision based on doing the best thing for their children that they have and for their family. And people are also commonly religious. //And the majority of people, like I said, are already parenting. And there really is no one type of person who accesses abortion. Abortion is very common. More common than most of us think. One in four people who can get pregnant in their life have an abortion. And even if you don't realize it, you probably know, love, and/or maybe even have a family member who has had an abortion. It's just much less commonly talked about. And so we think of it as something that's rare, but it's incredibly common.
Rhea Ramjohn: And that's right. Some of us might also be children of someone who's had an abortion. So I would like to follow up on that by asking what should people know about how they might not only physically feel but emotionally feel after an abortion?
Stephanie Frazin: That is such a great question and important to take into account how you're going to feel and how to anticipate how you're going to feel. But it's hard to tell. You know, people have a really wide range of emotions. The most common emotion, which 95% of people who have abortions report, is relief.
People sometimes feel happiness, sometimes feel sadness. There are a very small percentage of people that feel regret, but that's pretty rare. And I think it's important for us, less to predict exactly what you'll feel, but really to normalize that really different array of emotions that can happen just like in all different aspects of our lives and know that whoever you, you know, supports you during your abortion is also there after your abortion and you can always contact them. Or, there are other resources to really talk about emotions that may come up afterwards if you want more support or space to talk about those things.
Rhea Ramjohn: Mhmm. And what about physically? What happens to the body? Walk us through. I imagine our listeners are getting finally a chance to hear a very open conversation about abortion from an expert like yourself with a lot of experience. Help us understand. What can I expect, being there physically or what can I expect afterwards physically? How many days should I expect, maybe, to stay off of my feet or to anticipate certain, sort of, body aches? Does that happen?
Stephanie Frazin: So what people experience after an abortion can depend a little bit on what type of abortion they've had, either medication abortion or surgical abortion. But for all people there, it's really common to experience a certain amount of what we call period-like bleeding. It's not actually a period. It's just the cells that are remaining in the uterus passing out. And that can last up to a couple weeks, even sometimes three weeks, three weeks. But the bleeding shouldn't be much heavier than a period and often turns into spotting after about a week. People tend to experience some cramping afterwards, kind of a lower pelvic like uterus cramping, and that's usually relieved with heat or some type of NSAID. // And that cramping can last, you know, certainly in the first 24 hours. But it's very normal for it to last a few days and even up to a week. But it should progressively get better. Some risks of having abortions are things like infection. And if someone, you know, was having their pain totally resolved and then maybe a week later had a lot of pain, cramping, maybe a fever. Those would be warning signs for us that we'd want to definitely hear about and, and see them to be able to treat their infection.
Rhea Ramjohn: Right. We had a lot of questions from Clue users about what people feel after they have an abortion. So in your experience or in the literature, are there side effects or potential red flags that people should be on the lookout for?
Stephanie Frazin: Yeah. The most common complications of earlier abortions are things like infection. And signs of infection, // it would usually occur about five to seven days, sometimes longer, after an abortion has occurred. And those symptoms would include increasing pain in the lower pelvis, maybe a funny smelling odor or funny looking discharge, vaginal discharge, and having a temperature. Sometimes just over all, like body aches and pains at the same time can also be a sign of infection of the uterus. And those infections are easily treated with antibiotics that don't usually require any hospitalization or additional procedures. But if someone was experiencing those things after an abortion, we want to hear about it as soon as possible so that we'd be able to start treating an infection.
Rhea Ramjohn: This is a really important conversation, and I want to continue on this topic, but before we continue, we’re going to take a quick break.
Hormonal is brought to you by Clue. The period tracking app, and menstrual health encyclopedia, that takes YOUR cycle seriously.
And right now, we’re asking for your help. Clue needs your financial support to keep the lights on. You can do that by becoming a Clue plus subscriber. Your subscription not only keeps the work here at Clue going, but it also supports menstrual health research around the world, and protects data privacy.
Your subscription gives you access to our entire library of articles as well as new articles, app features, and curated content as they’re released.
For more on how to support the work and reap the benefits of becoming a Clue Plus subscriber, check out clue-dot-plus.
Alright, back to the show.
Rhea Ramjohn: You’re listening to Hormonal, I’m Rhea Ramjohn.
Ok Stephanie. I teased this a little bit already, but I actually have more listener questions for you. We reached out on Instagram and got a lot of responses, so I have some questions now.
We could only pick a few, but thanks to everyone for writing in. And I’m excited about this because I think these are questions that a lot of people have and don’t know who to turn to for trusted information.
Stephanie: Sure.
Rhea Ramjohn: So if you're if you're up for it, I would just run through about five questions, OK? Great. Thank you.
Rhea Ramjohn: All right. So Hannah asked us, how can different abortion methods affect your fertility in the future?
Stephanie Frazin: For a procedural abortion, a dilation and curatage, there is a very, very rare risk that by putting an instrument inside of the uterus that you could cause scar tissue to develop. The sort of scientific name for that is called Asherman syndrome. It is incredibly rare. It happens less than one percent of the time, but it is a risk that we review before doing the procedure and something that people should definitely know about before having the procedure.n terms of the way that it might affect things like other aspects of fertility. It doesn't change your hormones or or do anything other than that potential production of scar tissue that would affect future pregnancies.
Rhea Ramjohn: OK. And Karen wants to know, taking the abortion pill, what short or long term impact can it have on sexual health?
Stephanie Frazin That’s a good question, too. There's actually no research that shows that it changes. Sexual function, sexual health, certainly that, you know, that, when I say there's data or research, it just means somebody decided to do this study to look for that. And potentially no one has been choosing to do the study to look at a change in sexual function. I would say that. You know, for my own practice and experience outside of research, that sometimes people after they've had, you know, either a medication or surgical abortion, they may have a sense that they want to take some time before they start having sex again. And, you know, other people don't feel that way. There's a huge spectrum of what people feel, but it's not totally uncommon that people need to take some time before starting to have sex again, not physically, not that they would have a risk of infection or causing any physical harm, but for their, you know, just sensing what's right for them.
Rhea Ramjohn: One question that I think sometimes gets lost here, is that there are risks associated with being pregnant. It’s not like one of these options is risk free and the other is risk-full, so to speak, right?
Stephanie Frazin: It's really important when we talk about risk to also acknowledge that pregnancy itself is risky and it's actually much riskier to continue a pregnancy to full term than it would be to have an abortion and sort of introduce yourself to the risks that we just talked about. It's actually the the risk of, you know, even passing away from a pregnancy is about 14 times higher if you were to continue a pregnancy all the way versus having an abortion.
Rhea Ramjohn: Wow.
Stephanie Frazin: So when I talk to someone about risks, we have a very long and frank conversation about these things, so people can be well informed about their bodies. But I do start by making sure that they understand that these are things they need to know about, but they’re rare. And it’s actually safer than continuing their pregnancy.
Rhea Ramjohn: So Following up on that. One of our listeners, Liza, posted on isntragram, when is it unsafe to continue with an abortion?
Stephanie Frazin I can't actually think of a very good example of something that's unsafe. I would say specific instances could include if you're very sick from a respiratory illness. That's something that we'd want to support you in your recovery from that, before you received sedation for a procedural abortion, there's very specific certain reasons why we wouldn't recommend a medication abortion if you had a bleeding disorder or you were severely anemic. For someone like that, we would recommend that it would be safer for them to have the procedure in sort of a safer environment where they would have access to a blood transfusion or to other things that could help with their bleeding. But in general, it's, it's a pretty safe procedure. And most people can have an abortion.
Rhea Ramjohn: OK. Well, Stephanie, this is our last user question. And I’ve actually wondered about this too, so I’m happy that Sarah posted this question to us. Sarah asked: How does legalization of abortion historically affect abortion rates, birth rates and parental survival rates?
Stephanie Frazin: That's an excellent question. // In any context, we know that legalization of abortion saves lives, absolutely saves lives and allows for safe abortion. We can also see if we look at data now, you know, not in the 1970s, when we look at mortality in other countries where abortion is not legal, there's high mortality associated with unsafe abortion. You know, people for, not just in this last century, but for thousands of years, as soon as people could become pregnant, they found ways to end pregnancy. And now we have really safe ways to do that and to support people. And when we restrict those things, people will still end their pregnancy, they will still find a way. And that way is sometimes like self managed abortion, like we talked about with medications, can be really safe, but sometimes it's not. And sometimes people may not have access to those pills and are using other things or other methods that we know are unsafe. And it's another reason, you know, not just supporting people's bodily autonomy, you know, to make sure that we support them and that they don't want to be pregnant, but also to save lives, it's important to support decreasing restrictions to abortion access.
Rhea Ramjohn: You know often this kind of care is delivered at so called “women’s clinics” or similar limiting names. That’s a bit of a red flag for me, and makes me wonder, what should people who are perhaps not straight or they are not or do not present as cis women? What should they know about what it will be like for them to access abortion care?
Stephanie Frazin: Unfortunately, although there is definitely a movement in the community to have inclusive and supportive care, they may be experienced, have experiences like many obstetric and gynecological experiences for people who are trans or non binary, or do not present as a cis woman. They, they may experience discrimination, incorrect language and they may need to be really explicit to explain that what they're presenting for. And that is incredibly unfortunate that that is still occurring now. Um, unfortunately, I, as a cis-woman, it's hard for me to give advice, and I don't think it is my place to give advice to people who are going to experience that, because I am sure it would be traumatic, to…And then there's a certain trauma there in receiving medical care. But I think, I would say for any person who's, who's getting medical care, regardless of who they are, I think it's really important for them to advocate for themselves, which is much easier said than done.
Rhea Ramjohn: Right, and I think that’s important to acknowledge. You’re a cis woman, I’m a cis woman, and our understanding here is limited. But, I’m passionate about calling out for change to improve systems like these, so what would you say to our listeners who work in the medical field? What can they do to make their practices more inclusive or as inclusive as possible?
Stephanie Frazin: Yeah, I think some of the first things that are important to make practices inclusive is to make sure that when we come into contact with our patients, that we are asking them their pronouns, respecting their pronouns. Something important for me, I really only started doing the past four years is to try to stop using unnecessary language. So trying to omit the word woman from both my clinical work and my research, unless I see that a person or patient is wanting me to use that language, something that we're in the process of is changing the language of our clinics. So our general OB GYN clinic used to include women and now it's "obstetrics, midwifery and gynecology clinic" to be more inclusive, to take out the word woman. There's some really basic things that I think can also be helpful. Things like removing art or imaging that is only reflective of cis women and changing any documentation that patients are receiving// to have inclusive language that does not use the word woman.
Rhea Ramohn: Mhmm.
Stephanie Frazin I think some of the initial response, and I certainly had this as well, when people who are in obstetrics and gynecology or in any field that is providing reproductive health care. Because certainly it's not just OBGYNS, it may be internal medicine folks or family medicine folks, midwifery folks. But I think that the initial response is sometimes: “Well, I can't do that. Like, how can I talk about someone's period or how can I talk about pregnancy or abortion without using ‘woman.’” And it's actually much easier than it sounds, you can use terms like, “person with the ability to get pregnant” or “person at risk of an unintended pregnancy,” or there's just like a wide range of things that you can replace “woman” or “she” or sort of those gendered language. There's, there's. a lot of things, if you think about it and put the work in that can be used to to replace those.
Rhea Ramjohn Absolutely, I agree 100 percent. At Clue where we create the Hormonal podcast, when we started to talk about an episode on abortion and abortion access, immediately, there were questions and concerns about parts of the world where governments are making it harder to access abortion. How has abortion access changed in the last few years, and especially now that the COVID 19 pandemic has made practically everything more difficult?
Stephanie Frazin: You know, it is–the changes in abortion access are so nuanced, depending on where you are. There's locations like Oaxaca, Mexico where abortion is now going to be legal, and then there's places like right here in the United States where I am, where more and more restrictions are being passed to limit abortion care. And, I think in the pandemic, we see sort of like the baseline things that we hold true are just amplified. So for those who trust people and want to get them to access to abortion, we're all working harder and we're doing things to try to, you know, help people access what they need. And // at the same moment, the people who are trying to... who have always been trying to restrict access are just trying to loop that into the things that they're doing around COVID to try to restrict access more. You know, as someone who is supportive of people making their own choices for their body, I always think about, you know, why don't other people feel this way? Like how could you want to restrict someone's access to abortion and restrict someone's ability to make their own choices for themselves? And I wonder, you know, I feel like there is this righteousness that exists in both of us. Right? A righteousness on my part, in that people should do what they want with their bodies and this righteousness within people who want to restrict abortion. But. People who want to restrict abortion access. I feel like... they aren't seeing the people that I'm seeing. They aren't seeing them as people who are, you know, like we talked about before, people who are... have families and have lives and are thinking about what to do with their body and are being very thoughtful and caring for their family in choosing to have an abortion. And I'm always trying to think of ways in which, you know, what conversation could happen with those people that would help them see what I see. And that's that we really need to trust people with their reproductive choices and they know what's right for them. Whether it's in a pandemic or not, in a pandemic.
Rhea Ramjohn: Right.
Stephanie Frazin: And that that shouldn't you know, the pandemic shouldn't change those things, people should still be able to access this care and the service.
Rhea Ramjohn. Stephanie Frazin, joined us today from San Francisco, California. She’s a physician, researcher and family planning fellow and abortion expert at the University of California, San Francisco. Stephanie , thank you so much for speaking to us on Hormonal.
Stephanie Frazin: Thank you for having me. It's been a pleasure.
Credits
Hormonal is hosted by me, Rhea Ramjohn! Our Executive Producer is Kassandra Sundt.
Editorial help from:
Amanda Shea
Steph Liao
Nicole Leeds
Special thanks to:
Marta Pucci
Trudie Carter
Maddie Sheesley
Ryan Duncan
Aubrey Bryan
Claudia Taylor
Léna Calvarin
Lynae Brayboy
Mixing and recording help from Bose Park Productions and Rekorder Studios in Berlin.
Thanks for listening to Hormonal. Please rate and subscribe, and tell a friend! Until next time, I’m Rhea Ramjohn.
Related links:

Episode 2
October 19, 2020
The ABC: Abortion & Birth Control
What’s it like to get an abortion and the surprising ways the pandemic is changing abortion access.
About
1 in 4 people capable of getting pregnant will have an abortion in their lifetime. Despite this, finding accurate information about abortions is tricky. That’s why we’re exploring this topic and the stigma around it in our latest episode of Hormonal.
"The most common emotion, which 95% of people who have abortions report, is relief. People sometimes feel happiness, sometimes feel sadness. There are a very small percentage of people that feel regret, but that's pretty rare."
What’s it like to get an abortion and the surprising ways the pandemic is changing abortion access.
This episode of Hormonal is brought to you with financial support from Bayer. To learn more about Bayer’s support of Hormonal and other work here at Clue, check out helloclue.com/bayer.
On Hormonal, we explore the science behind hormones. But we also talk about society and the world around us. We know that there are lots of women who have periods and lots who don’t. We also know that there are people who aren’t women who have periods too. We also know we have listeners who have never had periods. We hope you feel welcome, even when a term that a guest uses maybe doesn’t apply to you.
At Clue, we believe that our identities are not determined by our bodies and we hope you feel welcome. Thanks for listening to Hormonal.
Rhea Ramjohn: Hi, I'm Rhea Ramjohn, and you're listening to Hormonal brought to you by Clue, the menstrual health app. This season, we’re focusing on birth control.
Birth control to me, and I’m sure to many people, is really about self determination. It’s about controlling my own body, and feeling empowered in that decision. In almost all cases, when we’re talking about birth control, we’re talking about preventing conception. Things like, condoms, the pill, and IUDs. These all prevent sperm from fertilizing an egg, and implanting in the uterus.
But what about what happens after a conception does take place? While most health care providers would not consider abortion a form of birth control, it does exist in this same universe of self determination and controlling our bodies. According to the Guttmacher institute and World Health Organization, there were on average 73 million abortions every year between 2015 and 2019.
And when performed properly, an abortion is one of the safest procedures out there. But politically and socially, there is still a stigma.
So today, we’re going to talk about what people should know about terminating a pregnancy, and how access is changing.
For more, we're joined by Stephanie Frazin from San Francisco, California. She's a physician, researcher and family planning fellow and abortion expert at the University of California, San Francisco. Stephanie, welcome to Hormonal.
Stephanie Frazin: Thanks for having me.
Rhea Ramjohn: So for this episode, we are not going to be talking quite so much about spontaneous abortions. Also known as miscarriages. We're going to be talking more about people who choose to terminate their pregnancies. Frazin, as I know you also like to be called in terms of options that are out there. There are medical and surgical abortions, correct?
Stephanie Frazin: Yes.
Rhea Ramjohn: Can you tell us how these work?
Stephanie Frazin: Yeah, sure. So I'll just tell you what an experience would be for someone who comes to see me in the clinic, who doesn't want to continue their pregnancy or is considering not continuing their pregnancy. When they first come, usually we'll chat with them about how far along that they think they are. And people who are less than 10 weeks along have the choice of either what we call medication abortion, or they have the choice of having a procedure which is sometimes called a dilation and curettage or a dilation and evacuation. If someone thinks that they want to have a medication abortion, we would walk them through what to expect and give them the pills for medication abortion, the first pill for medication abortion is called mifepristone. It's a very safe medication that works against the hormone progesterone, which is a hormone that we all have in our bodies and that supports pregnancy.
The second medications are ones that they'll take at home later. That medication is called misoprostol, and that medication can help actually pass the pregnancy. If someone was interested in a medication abortion. We would also chat with them about things to expect when they go home and take that misoprostol, which is typically someone starting to have bleeding and cramping, usually within six hours after taking the medication. But sometimes it takes up to 24 hours and that bleeding can be like a period, sometimes heavier than a period. And it kind of leads up to the point of passing the pregnancy and then becomes lighter after the pregnancy is passed. And that usually coincides with cramping,//which can be managed with maybe a heating pack, like Ibuprofen.
Rhea Ramjohn: Ok, you’ve mentioned early pregnancy options. And as a reminder to listeners, you’re talking about what to expect at your clinic, but experiences and regulations around gestational age can vary between countries and even states within the same country. Now, what about as the pregnancy progresses?
Stephanie Frazin: If someone presented to our clinic and were below the gestation of 24 weeks pregnancy, then they would have the option of having a surgical or procedural abortion. Below 14 weeks, that's called a dilation and curettage or D&C, and between 14 and 24 weeks, it's called a dilation and evacuation procedure. And if someone was interested in that, I would walk them through exactly what to expect for that procedure. And that, you know, the first thing that we do is set someone up kind of as if they were going to have a pap smear, laying with their back on a table and their feet up in stirrups. We then when they're ready, you know, at our clinic, we give the option for sedation. So, for a D&C procedure, people receive sedation and then they kind of guide us, do they want more sedation to be super sleepy or do they want to be less sleepy? And then we let them tell us when they're ready to start the procedure.
Past certain gestational ages will also have an anesthesiologist involved and they can give additional sedation until the person is sleepier and we always wait until either the person tells us that they're ready to start or they're asleep, depending on what our conversation has been beforehand. Then we'll place the speculum, which is that same kind of, metal or plastic device, that is placed in the vagina for things like pap smears or other gynecological exams. And once we place the speculum, we'll get the cervix in view, clean off the cervix. And then at our clinic, we do numbing medication around the cervix until we've tested to make sure that if the person is still awake that they're comfortable and if they're not comfortable, we take more time to do more numbing medication until they feel like they're ready to start. And then we'll dilate the cervix to the appropriate amount. And the cervix is kind of this you know, it's this closed door between the vagina and the uterus. And so we gently open it with dilators that go up in size. And then once we reach the appropriate size, we enter, we introduce this little straw into the uterus and that straw is then attached to suction and is used to perform the abortion.
Rhea Ramjohn: Can you tell me, is one type of abortion more common than the other?
Stephanie Frazin: Yeah. In the United States, surgical abortion is more common than medication abortion, but medication abortion is growing in popularity for many different reasons. You know, some people choose to have medication abortions because they want to avoid having a surgical procedure. You did mention earlier that it's a very safe procedure and it is. But some people just would prefer to avoid having any instrumentation or any procedure on their uterus. Other reasons: sometimes people do it for privacy. They want to have a medication abortion in the safety and security of their home versus having it in a clinic. Other reasons why medication abortion is growing in popularity is, you know, some people feel that it feels more like a natural process. Although you are using medications, the process is very similar to if someone was experiencing a miscarriage. And the other reason why people are more commonly having medication abortions, especially right now, is because of restrictions in abortion access. And some people are even, you know, navigating the Internet and ordering medications over the Internet to be able to have a medication abortion at home without the support of a clinic or a doctor because they aren't able to access an abortion or even a medication abortion where they live.
Rhea Ramjohn: Ok, I’d like to follow up on that a little bit. Just framing it within our current times in COVID. Is that another reason why you believe the medical abortions are on the rise? That people are able to facilitate this process at home?
Stephanie Frazin: So, you know, the numbers of growing medication abortion were actually happening before COVID and going up from, you know, about 20% of people using medication for abortion previously, to the most recent was about 39% of abortions in the United States are with medication. We don't have numbers yet to see how that has changed during the pandemic. But I can tell you anecdotally, there have been more, of course, there have been more restrictions around abortion during the pandemic. And so more people we know, we just don't have an exact number, more people are accessing medication abortion, definitely. And that may be, there have been some very recent changes in restrictions around medication abortion, actually relieving some restrictions during the pandemic. Previously, that first medication that I had mentioned mifepristone, is controlled by something called the REMS criteria through the FDA. So the REMS criteria is something that controls that first medication that we talked about, mifepristone. And REMS criteria. It's kind of funny to look at the other things that it controls. It controls very toxic chemotherapeutic agents through the FDA, things that it would be unsafe for someone to touch or handle. So it's used to make sure that those medications are only given in a health care facility by a licensed provider. This also applies to mifepristone, not for safety reasons, because it's a very safe medication, but for political reasons to limit access to mifepristone for medication abortion.
Stephanie Frazin: Just two weeks ago, a judge ruled that this REMS criteria would not apply to mifepristone during the pandemic. So kind of hot off the press made this ruling that would make it so that we would be able to, as clinicians, mail the medication to people. And that way we could expand access to medication abortion for people all over the United States, even if they weren't able to physically access a provider in a clinic, which was the previous situation.
Rhea Ramjohn: Right. So, Stephanie, tell us who seeks abortions.
Stephanie Frazin: So I think each of us maybe has that thought in our mind of, you know, who is the type of person getting abortions. And as I became an abortion provider, I learned that there really is no stereotype there. There are all different people who are accessing abortion care. And the average person is someone who is already a parent and maybe making this decision based on doing the best thing for their children that they have and for their family. And people are also commonly religious. //And the majority of people, like I said, are already parenting. And there really is no one type of person who accesses abortion. Abortion is very common. More common than most of us think. One in four people who can get pregnant in their life have an abortion. And even if you don't realize it, you probably know, love, and/or maybe even have a family member who has had an abortion. It's just much less commonly talked about. And so we think of it as something that's rare, but it's incredibly common.
Rhea Ramjohn: And that's right. Some of us might also be children of someone who's had an abortion. So I would like to follow up on that by asking what should people know about how they might not only physically feel but emotionally feel after an abortion?
Stephanie Frazin: That is such a great question and important to take into account how you're going to feel and how to anticipate how you're going to feel. But it's hard to tell. You know, people have a really wide range of emotions. The most common emotion, which 95% of people who have abortions report, is relief.
People sometimes feel happiness, sometimes feel sadness. There are a very small percentage of people that feel regret, but that's pretty rare. And I think it's important for us, less to predict exactly what you'll feel, but really to normalize that really different array of emotions that can happen just like in all different aspects of our lives and know that whoever you, you know, supports you during your abortion is also there after your abortion and you can always contact them. Or, there are other resources to really talk about emotions that may come up afterwards if you want more support or space to talk about those things.
Rhea Ramjohn: Mhmm. And what about physically? What happens to the body? Walk us through. I imagine our listeners are getting finally a chance to hear a very open conversation about abortion from an expert like yourself with a lot of experience. Help us understand. What can I expect, being there physically or what can I expect afterwards physically? How many days should I expect, maybe, to stay off of my feet or to anticipate certain, sort of, body aches? Does that happen?
Stephanie Frazin: So what people experience after an abortion can depend a little bit on what type of abortion they've had, either medication abortion or surgical abortion. But for all people there, it's really common to experience a certain amount of what we call period-like bleeding. It's not actually a period. It's just the cells that are remaining in the uterus passing out. And that can last up to a couple weeks, even sometimes three weeks, three weeks. But the bleeding shouldn't be much heavier than a period and often turns into spotting after about a week. People tend to experience some cramping afterwards, kind of a lower pelvic like uterus cramping, and that's usually relieved with heat or some type of NSAID. // And that cramping can last, you know, certainly in the first 24 hours. But it's very normal for it to last a few days and even up to a week. But it should progressively get better. Some risks of having abortions are things like infection. And if someone, you know, was having their pain totally resolved and then maybe a week later had a lot of pain, cramping, maybe a fever. Those would be warning signs for us that we'd want to definitely hear about and, and see them to be able to treat their infection.
Rhea Ramjohn: Right. We had a lot of questions from Clue users about what people feel after they have an abortion. So in your experience or in the literature, are there side effects or potential red flags that people should be on the lookout for?
Stephanie Frazin: Yeah. The most common complications of earlier abortions are things like infection. And signs of infection, // it would usually occur about five to seven days, sometimes longer, after an abortion has occurred. And those symptoms would include increasing pain in the lower pelvis, maybe a funny smelling odor or funny looking discharge, vaginal discharge, and having a temperature. Sometimes just over all, like body aches and pains at the same time can also be a sign of infection of the uterus. And those infections are easily treated with antibiotics that don't usually require any hospitalization or additional procedures. But if someone was experiencing those things after an abortion, we want to hear about it as soon as possible so that we'd be able to start treating an infection.
Rhea Ramjohn: This is a really important conversation, and I want to continue on this topic, but before we continue, we’re going to take a quick break.
Hormonal is brought to you by Clue. The period tracking app, and menstrual health encyclopedia, that takes YOUR cycle seriously.
And right now, we’re asking for your help. Clue needs your financial support to keep the lights on. You can do that by becoming a Clue plus subscriber. Your subscription not only keeps the work here at Clue going, but it also supports menstrual health research around the world, and protects data privacy.
Your subscription gives you access to our entire library of articles as well as new articles, app features, and curated content as they’re released.
For more on how to support the work and reap the benefits of becoming a Clue Plus subscriber, check out clue-dot-plus.
Alright, back to the show.
Rhea Ramjohn: You’re listening to Hormonal, I’m Rhea Ramjohn.
Ok Stephanie. I teased this a little bit already, but I actually have more listener questions for you. We reached out on Instagram and got a lot of responses, so I have some questions now.
We could only pick a few, but thanks to everyone for writing in. And I’m excited about this because I think these are questions that a lot of people have and don’t know who to turn to for trusted information.
Stephanie: Sure.
Rhea Ramjohn: So if you're if you're up for it, I would just run through about five questions, OK? Great. Thank you.
Rhea Ramjohn: All right. So Hannah asked us, how can different abortion methods affect your fertility in the future?
Stephanie Frazin: For a procedural abortion, a dilation and curatage, there is a very, very rare risk that by putting an instrument inside of the uterus that you could cause scar tissue to develop. The sort of scientific name for that is called Asherman syndrome. It is incredibly rare. It happens less than one percent of the time, but it is a risk that we review before doing the procedure and something that people should definitely know about before having the procedure.n terms of the way that it might affect things like other aspects of fertility. It doesn't change your hormones or or do anything other than that potential production of scar tissue that would affect future pregnancies.
Rhea Ramjohn: OK. And Karen wants to know, taking the abortion pill, what short or long term impact can it have on sexual health?
Stephanie Frazin That’s a good question, too. There's actually no research that shows that it changes. Sexual function, sexual health, certainly that, you know, that, when I say there's data or research, it just means somebody decided to do this study to look for that. And potentially no one has been choosing to do the study to look at a change in sexual function. I would say that. You know, for my own practice and experience outside of research, that sometimes people after they've had, you know, either a medication or surgical abortion, they may have a sense that they want to take some time before they start having sex again. And, you know, other people don't feel that way. There's a huge spectrum of what people feel, but it's not totally uncommon that people need to take some time before starting to have sex again, not physically, not that they would have a risk of infection or causing any physical harm, but for their, you know, just sensing what's right for them.
Rhea Ramjohn: One question that I think sometimes gets lost here, is that there are risks associated with being pregnant. It’s not like one of these options is risk free and the other is risk-full, so to speak, right?
Stephanie Frazin: It's really important when we talk about risk to also acknowledge that pregnancy itself is risky and it's actually much riskier to continue a pregnancy to full term than it would be to have an abortion and sort of introduce yourself to the risks that we just talked about. It's actually the the risk of, you know, even passing away from a pregnancy is about 14 times higher if you were to continue a pregnancy all the way versus having an abortion.
Rhea Ramjohn: Wow.
Stephanie Frazin: So when I talk to someone about risks, we have a very long and frank conversation about these things, so people can be well informed about their bodies. But I do start by making sure that they understand that these are things they need to know about, but they’re rare. And it’s actually safer than continuing their pregnancy.
Rhea Ramjohn: So Following up on that. One of our listeners, Liza, posted on isntragram, when is it unsafe to continue with an abortion?
Stephanie Frazin I can't actually think of a very good example of something that's unsafe. I would say specific instances could include if you're very sick from a respiratory illness. That's something that we'd want to support you in your recovery from that, before you received sedation for a procedural abortion, there's very specific certain reasons why we wouldn't recommend a medication abortion if you had a bleeding disorder or you were severely anemic. For someone like that, we would recommend that it would be safer for them to have the procedure in sort of a safer environment where they would have access to a blood transfusion or to other things that could help with their bleeding. But in general, it's, it's a pretty safe procedure. And most people can have an abortion.
Rhea Ramjohn: OK. Well, Stephanie, this is our last user question. And I’ve actually wondered about this too, so I’m happy that Sarah posted this question to us. Sarah asked: How does legalization of abortion historically affect abortion rates, birth rates and parental survival rates?
Stephanie Frazin: That's an excellent question. // In any context, we know that legalization of abortion saves lives, absolutely saves lives and allows for safe abortion. We can also see if we look at data now, you know, not in the 1970s, when we look at mortality in other countries where abortion is not legal, there's high mortality associated with unsafe abortion. You know, people for, not just in this last century, but for thousands of years, as soon as people could become pregnant, they found ways to end pregnancy. And now we have really safe ways to do that and to support people. And when we restrict those things, people will still end their pregnancy, they will still find a way. And that way is sometimes like self managed abortion, like we talked about with medications, can be really safe, but sometimes it's not. And sometimes people may not have access to those pills and are using other things or other methods that we know are unsafe. And it's another reason, you know, not just supporting people's bodily autonomy, you know, to make sure that we support them and that they don't want to be pregnant, but also to save lives, it's important to support decreasing restrictions to abortion access.
Rhea Ramjohn: You know often this kind of care is delivered at so called “women’s clinics” or similar limiting names. That’s a bit of a red flag for me, and makes me wonder, what should people who are perhaps not straight or they are not or do not present as cis women? What should they know about what it will be like for them to access abortion care?
Stephanie Frazin: Unfortunately, although there is definitely a movement in the community to have inclusive and supportive care, they may be experienced, have experiences like many obstetric and gynecological experiences for people who are trans or non binary, or do not present as a cis woman. They, they may experience discrimination, incorrect language and they may need to be really explicit to explain that what they're presenting for. And that is incredibly unfortunate that that is still occurring now. Um, unfortunately, I, as a cis-woman, it's hard for me to give advice, and I don't think it is my place to give advice to people who are going to experience that, because I am sure it would be traumatic, to…And then there's a certain trauma there in receiving medical care. But I think, I would say for any person who's, who's getting medical care, regardless of who they are, I think it's really important for them to advocate for themselves, which is much easier said than done.
Rhea Ramjohn: Right, and I think that’s important to acknowledge. You’re a cis woman, I’m a cis woman, and our understanding here is limited. But, I’m passionate about calling out for change to improve systems like these, so what would you say to our listeners who work in the medical field? What can they do to make their practices more inclusive or as inclusive as possible?
Stephanie Frazin: Yeah, I think some of the first things that are important to make practices inclusive is to make sure that when we come into contact with our patients, that we are asking them their pronouns, respecting their pronouns. Something important for me, I really only started doing the past four years is to try to stop using unnecessary language. So trying to omit the word woman from both my clinical work and my research, unless I see that a person or patient is wanting me to use that language, something that we're in the process of is changing the language of our clinics. So our general OB GYN clinic used to include women and now it's "obstetrics, midwifery and gynecology clinic" to be more inclusive, to take out the word woman. There's some really basic things that I think can also be helpful. Things like removing art or imaging that is only reflective of cis women and changing any documentation that patients are receiving// to have inclusive language that does not use the word woman.
Rhea Ramohn: Mhmm.
Stephanie Frazin I think some of the initial response, and I certainly had this as well, when people who are in obstetrics and gynecology or in any field that is providing reproductive health care. Because certainly it's not just OBGYNS, it may be internal medicine folks or family medicine folks, midwifery folks. But I think that the initial response is sometimes: “Well, I can't do that. Like, how can I talk about someone's period or how can I talk about pregnancy or abortion without using ‘woman.’” And it's actually much easier than it sounds, you can use terms like, “person with the ability to get pregnant” or “person at risk of an unintended pregnancy,” or there's just like a wide range of things that you can replace “woman” or “she” or sort of those gendered language. There's, there's. a lot of things, if you think about it and put the work in that can be used to to replace those.
Rhea Ramjohn Absolutely, I agree 100 percent. At Clue where we create the Hormonal podcast, when we started to talk about an episode on abortion and abortion access, immediately, there were questions and concerns about parts of the world where governments are making it harder to access abortion. How has abortion access changed in the last few years, and especially now that the COVID 19 pandemic has made practically everything more difficult?
Stephanie Frazin: You know, it is–the changes in abortion access are so nuanced, depending on where you are. There's locations like Oaxaca, Mexico where abortion is now going to be legal, and then there's places like right here in the United States where I am, where more and more restrictions are being passed to limit abortion care. And, I think in the pandemic, we see sort of like the baseline things that we hold true are just amplified. So for those who trust people and want to get them to access to abortion, we're all working harder and we're doing things to try to, you know, help people access what they need. And // at the same moment, the people who are trying to... who have always been trying to restrict access are just trying to loop that into the things that they're doing around COVID to try to restrict access more. You know, as someone who is supportive of people making their own choices for their body, I always think about, you know, why don't other people feel this way? Like how could you want to restrict someone's access to abortion and restrict someone's ability to make their own choices for themselves? And I wonder, you know, I feel like there is this righteousness that exists in both of us. Right? A righteousness on my part, in that people should do what they want with their bodies and this righteousness within people who want to restrict abortion. But. People who want to restrict abortion access. I feel like... they aren't seeing the people that I'm seeing. They aren't seeing them as people who are, you know, like we talked about before, people who are... have families and have lives and are thinking about what to do with their body and are being very thoughtful and caring for their family in choosing to have an abortion. And I'm always trying to think of ways in which, you know, what conversation could happen with those people that would help them see what I see. And that's that we really need to trust people with their reproductive choices and they know what's right for them. Whether it's in a pandemic or not, in a pandemic.
Rhea Ramjohn: Right.
Stephanie Frazin: And that that shouldn't you know, the pandemic shouldn't change those things, people should still be able to access this care and the service.
Rhea Ramjohn. Stephanie Frazin, joined us today from San Francisco, California. She’s a physician, researcher and family planning fellow and abortion expert at the University of California, San Francisco. Stephanie , thank you so much for speaking to us on Hormonal.
Stephanie Frazin: Thank you for having me. It's been a pleasure.
Credits
Hormonal is hosted by me, Rhea Ramjohn! Our Executive Producer is Kassandra Sundt.
Editorial help from:
Amanda Shea
Steph Liao
Nicole Leeds
Special thanks to:
Marta Pucci
Trudie Carter
Maddie Sheesley
Ryan Duncan
Aubrey Bryan
Claudia Taylor
Léna Calvarin
Lynae Brayboy
Mixing and recording help from Bose Park Productions and Rekorder Studios in Berlin.
Thanks for listening to Hormonal. Please rate and subscribe, and tell a friend! Until next time, I’m Rhea Ramjohn.
Related links: