Illustration by Emma Günther
Uterine fibroids: Symptoms, causes and treatment
Uterine fibroids are more common than you think, but what do we know about them?

Top things to know:
Fibroids are non-cancerous growths that affect as many as 70–80% of women and people with cycles
They grow in response to the hormones progesterone and estrogen, but factors such as race, age, and genetics can make you more likely to develop them
Fibroids don’t often cause symptoms but if they do, the symptoms are typically pain and heavy bleeding
There are many ways to treat uterine fibroids which include medication, surgery, and non-surgical methods
Uterine fibroids are a common cause of heavy bleeding and pain. They most often develop during the reproductive years (from your first period until your last). Here’s how to know if you have fibroids.
What are uterine fibroids?
Uterine fibroids are abnormal growths of muscle tissue that form within or on the walls of the uterus (1). Fibroids are often described as benign tumors. Although the word tumor sounds scary, a benign tumor simply means a non-cancerous growth (2). You may see in medical literature that uterine fibroids are described as myomas or leiomyomas.
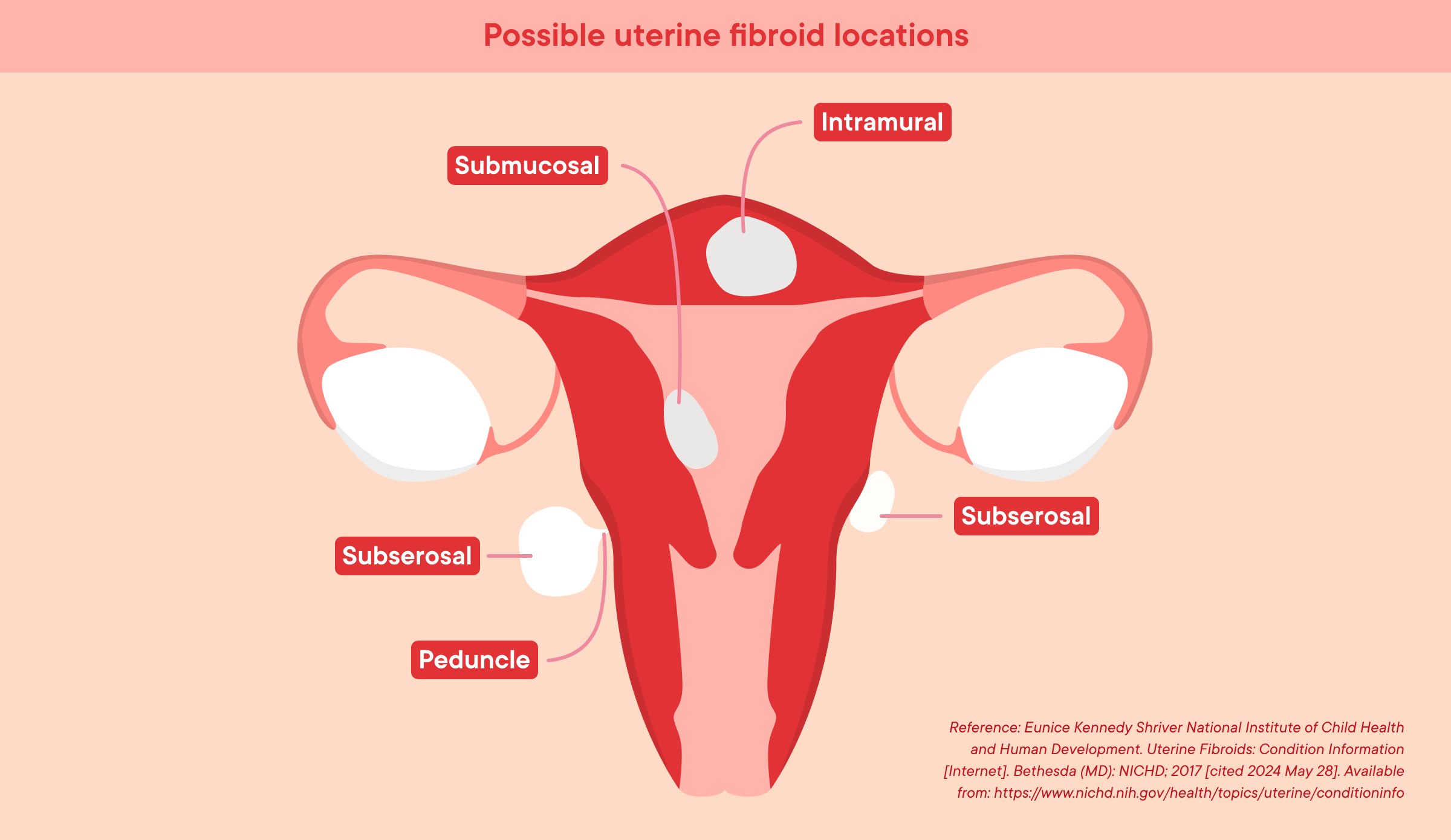
There are several types of uterine fibroids but the most common to know about are (3):
Intramural fibroids: These grow in the muscle wall of the uterus
Subserosal fibroids: These grow outside the wall of the uterus
Submucosal fibroids: Fibroids that start below the inner lining of the uterus and grow into the uterus
How common are uterine fibroids?
Uterine fibroids are very common. It is estimated that more than seven out of every ten women develop uterine fibroids by the time they reach menopause (4). They are more common in people of African descent, where it is thought that up to 80% of Black women may develop uterine fibroids (5). In reality, these numbers may be higher since most cases of fibroids do not cause any symptoms, so many people don’t know they have them (4). There is a lack of research on uterine fibroids in transgender and gender-diverse individuals, or those assigned female at birth. However, one resource suggests that the statistics are likely similar for anyone with a uterus (6). This highlights the need for research on gynecological conditions in gender-diverse people.
Fibroids are most common during the reproductive years, from puberty until menopause (7), and often shrink after menopause (8).
What are the common signs of uterine fibroids?
Some of the most common symptoms of uterine fibroids are (9):
Periods that are heavy, long, and painful
Pelvic pressure or pain
Pain during penetrative sex
Frequent urination
Constipation
Problems during pregnancy
Symptoms often depend on the size, location, and number of fibroids. For example, the fibroids that grow in the wall of the uterus (intramural fibroids), are more likely to cause infertility than those that grow outside of the uterus (subserosal fibroids) (10).
Rarely, uterine fibroids can cause more severe complications such as torsion (twisting of the fibroid), hemorrhage (very heavy bleeding), and degeneration (when the fibroid cells die, causing severe pain) (11). These complications need immediate medical treatment.
Research has shown that large fibroids, or multiple fibroids may cause a risk of early pregnancy miscarriage (12,13). Furthermore, large fibroids may cause complications later in pregnancy such as the need for cesarean section and preterm births (13). However, research on pregnancy and fibroids is limited, highlighting the need for further studies.
If you think you may have uterine fibroids, tracking your bleeding, pain, and any other symptoms with Clue can provide your healthcare provider with information that may help with diagnosis and in forming a treatment plan. You can report uterine fibroids in “My health record” with Clue. This helps us and researchers better understand people's experiences with and without these conditions. With research, we can improve healthcare for all people with cycles. Find out more about how we do research at Clue here.
What causes uterine fibroids?
The exact cause of uterine fibroids is not known. Research tells us that they develop when muscle cells in the uterus multiply too many times, which forms lumps of various shapes and sizes (14). These lumps can be numerous or few, in other words, some people have lots of fibroids and some people only have one. They can grow on both the inner and outer surfaces of the uterus and within the uterine wall.
The sex hormones estrogen and progesterone appear to play a role in the growth of uterine fibroids (15). This is likely why fibroids tend to shrink after menopause since the production of these hormones decreases (16).
New research shows that certain factors can cause muscle cells in the uterus to multiply abnormally (17,18). This means that some people are more likely to develop fibroids than others.
These factors include (17,19–20):
If you are over the age of 40 but have not reached menopause
If you are of African descent, with research suggesting that this is partly due to certain genetic factors
If you have high blood pressure or polycystic ovary syndrome (PCOS)
If you had your first period early
If you have low levels of vitamin D in your blood
Obesity
Consuming a diet high in red meat
What are the diagnosis and treatment options for uterine fibroids?
Most fibroids are diagnosed using a routine pelvic exam or ultrasound scan, however, sometimes further testing is required (21). Many people do not require treatment for fibroids if they don’t have symptoms or if the symptoms do not impact their daily lives. If your symptoms are severe, doctors may prescribe medication or recommend surgery (22).
How can a healthcare provider diagnose my uterine fibroids?
A healthcare provider will likely ask about your symptoms, as well as your medical and gynecological history. Some uterine fibroids can be diagnosed during a routine pelvic exam, while other diagnostic methods may include (21):
Transvaginal ultrasound: a sonogram, where a probe is placed into your vagina to look at your uterus
Abdominal ultrasound: a sonogram, where a probe is placed on your abdomen to look at your uterus
MRI: a type of scan that produces an image of your uterus
Sonohysterogram: an ultrasound performed after the uterus is filled with fluid
Hysteroscopy: a procedure where a small camera is inserted into your uterus through the vagina to visualize the uterus. This is done under local or general anesthetic.
How are uterine fibroids treated?
If fibroids are not causing unwanted symptoms, no treatment is usually necessary (23). Depending on the size, symptoms, and location, there are several ways to treat fibroids. These include medication, non-surgical methods, surgery, and lifestyle changes (24).
What kind of medication treats uterine fibroids?
Medical treatment options depend greatly on what symptoms you have. For example, paracetamol and ibuprofen are often used to manage pain (24). If you suffer from heavy bleeding, your doctor may prescribe you medication that helps reduce or stop the bleeding. These include (24):
Oral contraceptive pill: the combined hormonal birth control pill
Oral progestogen: a synthetic progesterone that helps reduce heavy periods
Tranexamic acid: a medication that helps your blood clot which reduces the amount of bleeding
Hormonal Intrauterine Device (IUD): a small T- shaped device placed at the top of your cervix
In some instances, your healthcare provider may also prescribe medication to reduce the size of your fibroids. These include (24):
Gonadotropin-releasing hormone analogues (GnRHas): a hormone that stops the ovaries from releasing estrogen and acts directly on the fibroid to decrease the size (25)
Ulipristal acetate: a medication that blocks the effects of progesterone (26)
It’s important to remember that these medications have side effects, and they are not suitable for everyone. Discuss the risks and benefits with your healthcare provider before starting them.
What are the surgical and non-surgical options for treating uterine fibroids?
When fibroids are still causing unwanted symptoms and medication has not helped, removing or destroying the fibroids through non-surgical and surgical routes may be an option. Some non-surgical options that you and your healthcare provider may consider are (27):
Uterine artery embolization: a procedure where the blood vessels that supply blood flow to the fibroid are blocked
Endometrial ablation: a minor procedure that removes the lining of the womb which helps with heavy bleeding and removes small fibroids
MRI-guided ablation: an MRI scan that uses laser or ultrasound energy to destroy the fibroid
Ultrasound-guided ablation: a newer technique that uses a sonogram and heat to destroy the fibroid
Sometimes, surgical procedures may be considered if other methods have not worked. Some options are (27):
Myomectomy: a surgery that removes certain types of fibroids from the uterus
Hysteroscopic resection of fibroids: a surgery that uses a small camera and instrument to remove the fibroid
Hysterectomy: a surgery that removes the uterus (only after other options have been unsuccessful)
Can you treat uterine fibroids with lifestyle changes?
Although there is little evidence that lifestyle changes can shrink or remove fibroids, a recent study suggests they may help reduce the risks and severity. Changes such as eating less red meat, consuming a balanced diet with plenty of fruits and vegetables, minimizing stress, and reducing alcohol intake may all be beneficial (28). One study also suggests that exposure to chemicals in plastics called phthalates may increase the risk of fibroids (29). More research is needed in this field, but reducing your plastic use could be a positive step. It’s a great way to care for your body and the environment at the same time.
What happens if I don’t get my uterine fibroids treated?
The good thing is that the majority of uterine fibroids do not require any treatment as they do not cause symptoms (30). Sometimes the pain and bleeding they cause is manageable. In such cases, using over-the-counter pain medication may be enough to manage the pain (31). If your fibroids cause heavy bleeding, and they are left untreated they could cause anemia (32), a condition where the body has insufficient healthy red cells in the blood to carry oxygen to vital organs. Furthermore, some research suggests that leaving fibroids that cause infertility untreated may affect your chances of becoming and staying pregnant (33). Ultimately, it is your body, and the treatment option you choose with your healthcare professional should be the one that works best for you.
FAQs
What are the main causes of uterine fibroids?
Research indicates that uterine fibroids are caused when muscle cells in the uterus multiply, forming abnormal growths. This is usually due to progesterone and estrogen. Several factors make you more likely to develop fibroids such as age, race, genetics, and when you had your first period (34).
Can dietary changes help manage symptoms of uterine fibroids?
More research is needed into diet, fibroids, and their symptoms; however, some studies show that increasing your intake of fruit and vegetables and limiting red meat may help reduce the risk of developing fibroids (28,35).
Can uterine fibroids affect pregnancy?
Research suggests that certain types of fibroids can affect fertility and cause early pregnancy miscarriage (3,10,33), often when they are very large. If you have fibroids and are struggling with fertility you can speak to your healthcare provider about treatment options.
What is the difference between uterine fibroids and uterine polyps?
Both uterine fibroids and polyps are abnormal growths. However, fibroids are benign growths of the muscular layer of the uterus whereas uterine polyps are growths of the endometrial layer. Unlike fibroids, polyps are more likely to cause symptoms and can be malignant cancers (36,37).
